Cholera: symptoms, causes, methods of treatment and prevention. Cholera
Story
Cholera is the oldest human disease that spread to many countries of the world and even continents and claimed millions of human lives. The endemic focus of cholera was the basins of the Ganges and Brahmaputra rivers in India. The combination of a hot climate with an abundance of rainfall, geographical features (low terrain, many floodplains, canals and lakes) and social factors ( high density of the population, intensive pollution of water bodies with faeces, the use of polluted water for drinking and domestic needs) determined the rooting of this infection in this region.
Until 1960, there were six known cholera pandemics, although they were practically not separated by epidemically prosperous periods. The first cholera pandemic, which began in India in 1817, in the next 8 years was brought to Ceylon, the Philippines, China, Japan and Africa, then to Iraq, Syria and Iran, and finally to the cities of the Caspian basin of Russia (Astrakhan, Baku) . The second cholera pandemic (1828-1837), which also began in India, spread to China, from where by caravan routes to Afghanistan and Russia (Bukhara, Orenburg). Another route for cholera to enter Russia is through Iran, from where it spread to the countries of the Middle East and Transcaucasia. In this pandemic, cholera swept most of the provinces of Russia, was brought to Western Europe and North America. The third cholera pandemic (1844-1864) began with epidemics in India, China, the Philippines, Afghanistan and spread through the countries of Central Asia and Iran to the Transcaucasus. The penetration of cholera into Russia was associated with an epidemic that broke out in the countries of Western Europe, from where the infection was also brought to North America. The fourth cholera pandemic (1865-1875) began in India and, moving east (China, Japan) and west, reached Europe, Africa and America. In this pandemic, cholera entered Russia through Turkey and from the west through Prussia. The fifth cholera pandemic (1883-1896), which engulfed the same districts of Asia, the southern ports of Europe and America, did not bypass Russia either. The sixth cholera pandemic (1900-1926) was characterized by a pronounced second rise, which is associated with wars (Balkan, World War I, as well as with intervention and civil war in Russia).
In the periods between the described pandemics and after 1926, in some Asian countries there was not a year free from an epidemic rise in the incidence. Existing statistics are based mainly on the number of deaths from cholera. So, in China in 1939-1940, more than 50 thousand people died of cholera. According to official Some 10 million people died of cholera in India between 1919 and 1949. After 1950, there was a marked decrease in the spread of cholera.
If from 1919 to 1949, according to the generalized data of O. V. Baroyan (1970), 350-400 thousand people died annually from cholera, then in the period from 1950 to 1954 this figure was 77 thousand, and in the next five years - approximately 40 thousand. Classical cholera remained only in the ancient endemic focus (in India) and in the 70s of the 20th century did not manifest itself as massive epidemics. The pandemic spread of cholera in these years is associated with a new pathogen - the biovar El Tor. The pronounced ability of the El Tor biovar to cause cholera epidemics attracted the attention of specialists as early as 1937, when in Indonesia on about. Sulawesi experienced an epidemic of cholera caused by the specified pathogen. Mortality in this epidemic was 50-60%.
The widespread occurrence of El Tor cholera began in 1961, which many researchers consider the start of the seventh cholera pandemic. Assessing the current situation, the WHO Expert Committee (1970) considered it quite likely that cholera would spread in the near future and appear in those parts of the world in which it had been absent for many years. The role of biovar El Tor as an etiological factor in cholera rapidly increased; the number of diseases caused by this pathogen has reached epidemic proportions. So, in 1960, the biovar El Tor was detected in 50%, and in the following year - in more than 80% of all cases of cholera. Even in India in the 70s of the 20th century, the biovar El Tor occupied a predominant position.
According to far from complete official data, in 1961 cholera epidemics were registered in 8-10 countries; in the next four years, 18 countries were covered by cholera, and from 1965 to the beginning of 1970, 39 countries of the world. Such a rapid spread of cholera in many countries of the world was not observed in any of the previous pandemics. At the same time, the initial appearance of infection in many countries did not end with the elimination of the epidemic focus and the establishment of complete epidemic prosperity. Cholera took root in these countries. The developing pandemic of El Tor cholera also covered those countries where the disease was either not recorded for many years, or was absent throughout the history of previous pandemics.
First, El Tor cholera appeared on about. Sulawesi, then to Macau and Hong Kong, from where it was brought to Sarawak, and by the end of 1961 to the Philippines. In the next 4 years, El Tor cholera appeared on about. Taiwan, penetrated into the countries of Southeast Asia and then to South Korea. In 1964, the El Tor cholera epidemic originated in South Vietnam, where about 20,000 people fell ill. By 1965, it had reached Afghanistan and Iran, spreading in areas immediately adjacent to the borders of the USSR. The final northwestern border of the spread of cholera in mid-1965 was an epidemic outbreak in the Karakalpak ASSR and the Khorezm region of the Uzbek SSR. The further development of the El Tor cholera pandemic is characterized by the repetition of epidemic outbreaks in the countries of Southeast Asia, the Near and Middle East and its penetration into the African continent. In 1970, epidemic outbreaks of El Tor cholera arose in Odessa, Kerch, and Astrakhan.
The climax of the seventh cholera pandemic is 1971. If in 1970 there were 45,011 cholera patients in the world, then in 1971 - 171,329 patients, in 1972 - 69,141, in 1973 - 108,989, in 1974 - 108,665 and in 1975 - 87,566 patients. In 1971, 102,083 cases of cholera were registered in Asian countries; the highest incidence was observed in India, Indonesia, Bangladesh and the Philippines. In Africa, 69,125 cases of cholera were reported; while the highest incidence was in Ghana, Nigeria, Chad, Niger, Mali, Morocco, Cameroon, Upper Volta.
In 1971, El Tor cholera was also registered in some European countries: Portugal, Spain, France, Sweden and others. The concept was seriously shaken that El Tor cholera is a disease only of developing countries in which the sanitary and hygienic standard of living of the population has not reached the optimum preventing the development of an epidemic. This concept was even more shaken by the cholera epidemic that arose in 1973 in Naples (Italy) - over 400 cases of diseases; the epidemic was associated with the consumption of oysters harvested in the coastal waters of the Mediterranean Sea.
In subsequent years, epidemic rises in the incidence of El Tor cholera were observed in 36-48 countries: in 1976, 66,804 cases were registered, in 1977, 58,661, in 1978, 74,632, and in 1979, 54,179.
The accumulated data characterizing the features of El Tor cholera do not fit into the concepts of modern epidemiology, which considers the epidemic process as a series of passages of the pathogen from the carrier to a healthy person. At the same time, environmental objects (water from open reservoirs, sewer discharges) are assigned the role of transmission routes that bring the pathogen to the human body. According to these well-established ideas, a person is the only object that maintains the continuity of the epidemic process. This provision excludes the existence (not temporary preservation, but development and accumulation) of the causative agent of El Tor cholera in the environment outside the human body. An analysis of the epidemic situation on cholera that had developed by the 1970s in various countries of the world shows that the difference in the timing of the onset of epidemics in these countries is several days, and this is not enough to form a focus and consistently progressively move cholera from the territory of one country to the territory of another. . Theoretically, it can be assumed that sometime in the past the population of these countries (including those in which cholera did not occur throughout their history) was simultaneously infected, and under some currently unknown conditions in 1970 and then in In 1971, epidemics arose in them at the same time. It is difficult to say whether these unknown conditions are determined only by migration processes.
The epidemic situation of cholera in the world remains tense. In countries such as India, Indonesia, Burma, Bangladesh, Malaysia, the Philippines, Ghana, Cameroon, Niger, Nigeria, Senegal and others, there are ongoing cholera epidemics with annual registration of patients from hundreds to several thousand people.
Etiology
The causative agent of cholera is Vibrio cholerae Pacini 1854. There are two biovars: classic - Vibrio cholerae biovar cholerae and El Tor - Vibrio cholerae biovar eltor. Both biovars form serogroup 01.
The causative agent of cholera was first discovered in Italy. pathologist F. Paniki in 1854 in the contents of the intestines and the mucous membrane of the small intestine of people who died of cholera in Florence. In 1883 in Egypt
R. Koch isolated vibrio cholerae in pure culture from the feces of cholera patients and the corpses of those who died from cholera and studied its properties. Gotschlich (F. Gotschlich) in 1906 at the El Tor quarantine station (in Egypt, on the Sinai Peninsula) isolated from the intestines of pilgrims a vibrio in biological properties the same as that isolated by R. Koch, but differing in hemolytic properties. For a long time it was not considered the causative agent of cholera. Only in 1962, in connection with the seventh cholera pandemic caused by vibrio El Tor, was it recognized as the causative agent of cholera.
Over the years, researchers have discovered and described vibrios, some of which are similar in biochemical properties to Vibrio cholerae, but differ in somatic O-antigen (see the full body of knowledge: Bacteria, antigens of bacteria) and are not the causative agents of cholera. They were called cholera-like vibrios, and later NAG vibrios (non-agglutinating vibrios). Based on the similarity of the DNA structure and the commonality of many biological characteristics, they are also assigned to the species V. cholerae. Thus, the species V. cholerae is divided according to the structure of the somatic O-antigen into serogroups, of which the causative agent of cholera is V. cholerae 01, and V. cholerae 02; 03; 04 ... up to 060 and more can cause banal enteritis and gastroenteritis.
V. cholerae 01 is represented by serotypes (serovars) of Ogawa, Inaba, and Gikoshima. Vibrio cholerae produces exoenterotoxin - cholerogen, which is obtained in its pure form and is a protein with a relative mol. weighing (weighing) 84,000, consisting of 2 immunologically different fragments.
Animals do not suffer from cholera under natural conditions; during experimental infection, suckling rabbits are most susceptible to cholera infection.
The place of reproduction of the causative agent of cholera is the human intestine. Nevertheless, it can survive in the environment for a certain period of time, and under favorable conditions, it can multiply, which is especially true for the El Tor biovar. It is suggested that some atypical (not producing or weakly producing exotoxin - cholerogen) El Tor vibrios are free-living microorganisms.
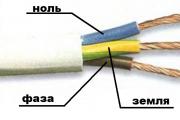
Vibrio cholerae are small, slightly curved or straight polymorphic rods 1.5-3 micrometers long, 0.2-0.6 micrometers wide, do not form spores and capsules, have one polarly located flagellum, 2-3 times longer than the size cells, which determines the active mobility of the vibrio (see figure). They stain well with aniline dyes and are gram-negative. An electron microscopic study showed a complex cellular structure of vibrios, characteristic of gram-negative bacteria. Vibrio cholerae are facultative anaerobes; they grow well on ordinary nutrient media of a slightly alkaline and alkaline reaction, especially if they contain sodium chloride at a concentration of 0.5-2%; optimal pH 7.6-8.2. Microbes grow at t° 10-40° (temperature optimum 35-38°).
In meat-peptone broth and 1% peptone water, the microbe multiplies rapidly: after 3-4 hours, cloudiness appears on the surface, and a little later, a delicate film. On alkaline agar, after 14-16 hours at t ° 37 °, Vibrio cholerae forms medium-sized, smooth, transparent colonies with a bluish tint, the surface of the colonies is moist, shiny, and the edge is even.
Vibrio cholerae forms oxidase, decarboxylates lysine and ornithine and does not decompose arginine, breaks down glucose under aerobic and anaerobic conditions with the formation of acid without gas, which is characteristic of the entire genus Vibrio. Vibrio cholerae also ferment mannitol, maltose, sucrose, mannose, levulose, galactose, starch and dextrin, do not break down arabinose, dulcitol, raffinose, rhamnose, inositol, salicin and sorbitol; produce indole from tryptophan and reduce nitrate to nitrite. Vibrio cholerae belongs to group I according to Heiberg (see the full body of knowledge: Vibrios) - it decomposes sucrose and mannose and does not decompose arabinose. Possessing a pronounced proteolytic activity, it liquefies gelatin, casein, fibrin and other proteins. It produces lecithinase, lipase, RNase, mucinase, neuraminidase. Vibrio cholerae of the El Tor biovar, when grown in Clark's glucose phosphate broth, as a rule, form acetylmethylcarbinol, while Vibrio cholerae of the classical biovar do not possess such an ability. Some strains of biovar El Tor lyse sheep and goat erythrocytes in a liquid nutrient medium.
The antigenic structure of both biovars of the causative agent of cholera is the same. They contain a thermostable somatic antigen 01. By the method of double diffusion precipitation in the gel, 7 antigens were found in the extract of Vibrio cholerae - from α to Θ. The most studied is the thermostable lipopolysaccharide a-antigen of the cell wall, which determines the serological specificity. This antigen also has the properties of an endotoxin and, when administered parenterally, causes the production of antibodies, providing antibacterial immunity. The thermolabile flagellar H-antigen is the same in representatives of all V. cholerae serogroups.
Vibrio cholerae is sensitive to an increase in temperature: at t ° 56 ° it dies after 30 minutes, and at t ° 100 ° - instantly. It tolerates low temperatures relatively well, remaining viable at t ° 1-4 ° for at least 4-6 weeks. High sensitivity to drying and sunlight, to disinfectants, including alcohol, carbolic acid solution and especially to acids.
Vibrio cholerae is highly sensitive to most antibiotics - tetracyclines, chloramphenicol, rifampicin; sensitive to erythromycin, aminoglycosides, broad-spectrum semi-synthetic penicillins, somewhat less sensitive to cephalosporins.
Morphological, cultural and biochemical characteristics of cholera vibrio and non-agglutinating vibrios are the same.
Identification of cholera vibrios is based on the determination of a specific somatic 01-antigen and sensitivity to cholera phages: the classical biovar - to the C phage, and the El-Tor biovar - to the El-Tor phage. Biovars are also identified by sensitivity to polymyxin (classic biovar - sensitive, El Tor biovar - resistant); hemagglutination of chicken erythrocytes (classic biovar does not cause hemagglutination, El Tor biovar does); production of acetylmethylcarbinol (classic biovar does not produce, biovar El-Tor produces more often).
Epidemiology
The source of infection is a person - a patient and vibrio carrier. In cholera, vibrio-carrying is observed after an illness, erased and atypical forms are often found, as well as healthy vibrio-carrying (see the full body of knowledge: Carrying infectious agents). The pronounced resistance of El Tor vibrios to the effects of adverse environmental factors should also be taken into account.
According to prevailing views, the basis for the occurrence of epidemic outbreaks of cholera, as well as the persistence of the pathogen in the inter-epidemic period, is determined by its constant circulation among the population. This circulation appears either as a direct transmission of the pathogen to a healthy person from the patient, that is, the disease is accompanied by further transmission of the infection (possibly in the absence of measures to isolate the diseased), or in the form of the appearance of erased forms of the disease, as well as carriage, which are links between clinically pronounced forms, or as a chain of carriers that fills the period between two epidemic outbreaks of the disease. According to these ideas, the pathogen can only temporarily persist in the environment, for example, in the ice of rivers and lakes.
However, the data obtained in the study of El Tor cholera epidemics in the 70s significantly expanded the understanding of the epidemic process in this infection. El Tor cholera outbreaks begin against the background of El Tor vibrio contamination of open water bodies contaminated by sewage. Attempts to clarify the beginning of the current epidemic situation by checking the medical records of hospitals and clinics in order to identify the first case of cholera, as well as mass serological studies to detect antibodies to vibrios in those who suffered from intestinal disorders in the past, have never given positive results.
The possibility of direct infection of a healthy person from a patient or carrier (the so-called contact route), as with any intestinal infection, is not excluded. However, this mechanism of infection, with a well-established system for identifying and urgent hospitalization (isolation) of a sick person, loses its leading significance. With El Tor cholera, individual patients who did not communicate with each other are often registered in a locality at the same time or within a few days (usually after weekends in the summer). But the examination reveals that the infection of all patients is associated with open water bodies (bathing, fishing), polluted by sewage. The existence of the vibrio El Tor, independent of a person, was first established by the studies of O. V. Baroyan, P. N. Burgasov (1976) and others. According to their data, in the Astrakhan region. in an open reservoir, isolated from a person's dwelling and its sewage discharges, for 2 years (observation period), El Tor vibrios of the Ogawa serotype were constantly detected (in the absence of diseases associated with this serotype in the past). The role of the environment is also eloquently evidenced by the above-mentioned El Tor cholera outbreak in Naples (1973), caused by eating oysters infected with El Tor vibrios. The data of P. N. Burgasov on the findings of El-Tor vibrios in hydrobionts, on the intensive reproduction of vibrios when they are directly introduced into polluted river water or into bath sewer waters give grounds to assert that the environment (primarily hydrobionts of open water bodies) can be not a place of temporary residence of El Tor vibrios, but their habitat, reproduction and accumulation.
Numerous observations of foreign and domestic researchers do not always agree in assessing the timing and epidemic significance of vibrio carriers. To a certain extent, this is explained by the fact that the observational data refer to both classical cholera and cholera caused by the biovar El Tor. So, L. V. Gromashevsky and G. M. Vaindrakh (1947), as a result of summarizing a large amount of material, note that usually the intestines of a person who has been ill with cholera is cleared of cholera vibrios by the 15th - 20th day from the onset of the disease and only in 1% cases, the pathogen is detected after 1 month. Cases of carriage for 8-9 months are extremely rare (one in several thousand cholera patients). The possibility of long-term carriage by healthy people of cholera vibrios L. V. Gromashevsky calls into question. This judgment is consistent with the data of V. I. Yakovlev (1892 - 1894), S. I. Zlatogorov (1908 - 1911), G. S. Kulesha (1910) and others. According to WHO experts Barua and Tsvetanovich (D. Barua, V . Cvjetanovic, 1970), carriers of cholera vibrios represent the main danger of importing cholera to countries where it has not previously been recorded. It is assumed that it is the carriers that retain V. cholerae in the inter-epidemic period. However, as a result of a unique experiment conducted on the territory of our country, when 3 million 800 thousand healthy people were examined for vibrio carrying (and a number of contingents were even examined again), not a single carrier of cholera vibrios was detected, which contradicts the conclusions of WHO experts.
Other data were obtained during the study of this issue in the 70s of the 20th century in the foci of cholera El Tor. According to materials summarized by Barua and Tsvetanovic (1970), the ratio of the number of carriers to the number of patients ranges from 10:1 to 100:1. Such a striking difference in the data on the frequency of the formation of a healthy carrier in epidemic foci of cholera requires additional and very well-reasoned verification. However, it must be taken into account that the data on the frequency of vibrio-carrying, given by Barua and Tsvetanovich, are mainly based on the materials of studies conducted within the limits of endemic foci of cholera, where the intensity of the epidemic process is extremely high. It is also possible that patients with erased forms of the disease are often included in the number of vibrio carriers. The main reasons for the widespread contamination of the causative agent of cholera in large groups and the appearance in connection with this of a significant number of patients with asymptomatic forms or healthy carriers in many countries that are unfavorable for cholera are the insufficiency and limited measures to combat it. For example, speaking of moderate diarrhea, Mondal and Zak (Mondal, R. B. Sack, 1971) note that it is of great epidemiological importance, since it contributes to the persistence of the pathogen among the population, but does not represent a clinical problem, since it often does not recognized and not treated.
The mechanism of transmission of the causative agent of cholera to humans, as well as the mechanism of transmission of other intestinal infections(see the full body of knowledge: The mechanism of transmission of infection), is the penetration of cholera vibrios into the gastrointestinal tract with contaminated water or food. However, the possibility of infection through direct contact with the patient, when the pathogen can be brought into the mouth by hands contaminated with the secretions of the patient with cholera or a vibrio carrier, as well as the transmission of cholera pathogens by flies, is not excluded.
Due to the fact that environmental factors are important elements of the pathogen transmission mechanism from a patient (or carrier) to a healthy one, the degree of its impact on vibrios and the resistance of the latter is essential. Ceteris paribus, the El Tor vibrio has a greater ability to survive outside the human body than the classic cholera vibrio. The resistance of the pathogen depends on the characteristics of the habitat, in particular on its contamination with other microflora, the concentration of salts, carbohydrates and organic substances in it, as well as on the temperature and pH of the environment. Disinfectants used in the practice of combating intestinal infections in normal concentrations have a detrimental effect on cholera vibrios. Direct sunlight has the same effect. Studies by Barua et al. (1970) on the survival of cholera vibrios on various food products showed that attempts to isolate vibrios from a wide variety of vegetables and fruits bought at markets located in endemic foci of cholera were made repeatedly, but without success.
As for the survival of Vibrio El Tor on artificially seeded products, its period at room temperature in relation to meat and fish products, as well as vegetables, is 2-5 days. These data were obtained in the Philippines in 1964. Research by P. N. Burgasov and others (1971, 1976), carried out when deciding on the possibility of exporting vegetables and watermelons from cholera-affected areas, found that at a daytime air temperature of 26-30 ° and In diffused sunlight, tomatoes and watermelons artificially seeded with El Tor vibrio were free from it after 8 hours. The greatest danger regarding the spread of cholera is the water of open polluted reservoirs (rivers, lakes, water areas of ports and beaches), as well as damaged water pipes and wells.
Observations of the survival of Vibrio cholerae El Tor in open water contaminated by sewer discharges indicate the long-term survival of the pathogen in this environment, which is of great epidemiological significance. These periods are calculated in several months, and when the temperature drops and the reservoir freezes, vibrios can overwinter. Sewer discharges of large cities are characterized by optimal temperature conditions for the pathogen and a neutral or alkaline reaction as a result of widespread use by the population hot water and detergents. According to P. N. Burgasov (1976), after a single discharge of acids into the sewer system industrial enterprise, which changed the reaction of sewer water to pH 5.8, vibrios, which for a long time were found in water samples taken below the city sewer discharge, were no longer found.
The formation and development of a cholera epidemic, its scale is determined by the presence of patients or vibrio carriers, the conditions of possible infection of environmental objects (water, food products) with their feces, the possibility of direct transmission of the pathogen from a patient (carrier) to a healthy one, as well as the effectiveness of epidemiological surveillance and the timeliness of anti-epidemic measures. . Depending on the predominance of certain factors of transmission of infectious agents, emerging epidemics are peculiar both in terms of the dynamics of the appearance and growth of diseases, and in terms of the effectiveness of anti-epidemic measures. For example, the waterway of cholera spread is characterized by a sharp (within several days) rise in the incidence, which leads to massive infection of the environment and a significant increase in the risk of infection of people in the area. Naturally, the exclusion of the water factor in the spread of cholera (neutralization of water, the prohibition of swimming in reservoirs infected with the pathogen) stops the rise in the incidence, but a tail of single diseases remains due to other ways of transmitting the infection.
A characteristic feature of the formation of El Tor cholera foci is the occurrence of severe forms of the disease against the background of well-being for intestinal infections in the area. Moreover, during previous bacteriological examinations of environmental objects and patients with intestinal disorders, cholera pathogens were not detected. Retrospective studies of survivors of intestinal infections also ruled out cholera in their history.
During the cholera outbreak of the 1970s, older patients predominated in our country, and children's diseases were an exception. In endemic areas of other countries of the world, mainly children are ill, and people of older age groups have immunity to cholera acquired during their life in these areas.
Pathogenesis
Vibrio cholerae enter the human body through the mouth along with contaminated water or food. If they do not die in the acidic environment of the contents of the stomach, then they enter the lumen of the small intestine, where they multiply intensively due to the alkaline reaction of the environment and the high content of protein breakdown products. The process of reproduction and destruction of cholera vibrios is accompanied by the release of a large amount of toxic substances. So, the exotoxin of cholera vibrios (cholerogen), applied to the mucous membrane, causes a whole cascade of biochemical changes in cells; the cycle of these changes is not fully understood. The most important is the activation of adenylate cyclase in the enterocytes of the small intestine, which leads to an increase in the synthesis of cyclic 3-5-adenosine monophosphate, the level of which determines the volume of secretion of intestinal juice (see the full body of knowledge: Intestine). The leading link in the pathogenesis of cholera is the development of acute isotonic dehydration (see the full body of knowledge: Dehydration of the body), accompanied by a decrease in the mass of circulating blood (hypovolemia), hemodynamic disorders and disorders of tissue metabolism. Hypovolemia, a drop in blood pressure and metabolic acidosis lead to the development of acute renal failure, disruption of cardiac activity and the function of other organs, as well as blood clotting processes (an increase in fibrinolytic and anticoagulant activity of the blood). In addition to dehydration, a significant role is played by the loss of essential electrolytes during vomiting and diarrhea, primarily potassium (see the full body of knowledge: Hypokalemia), as well as sodium and chlorine. The loss of potassium in cholera can reach 1/3 of its content in the body, and in case of insufficient replenishment, it leads to impaired myocardial function, damage to the renal tubules, as well as intestinal paresis and severe muscle weakness.
In accordance with the clinical and pathogenetic classification of cholera proposed by V. I. Pokrovsky and V. V. Maleev (1973), there are four degrees of dehydration of the body, respectively, fluid loss as a percentage of body weight (mass): I degree - 1-3% ; II degree - 4-6%; III degree - 7-9%; IV degree - 10% or more. Dehydration of the I degree does not cause noticeable physiological disturbances. Dehydration of the II degree is accompanied by the appearance of moderately pronounced signs of dehydration. Dehydration of the III degree is characterized by the presence of the entire symptom complex of dehydration and the state of unstable compensation of water and electrolyte balance. With IV degree dehydration (algidic period, algid), secondary changes in the most important systems are noted and, as a result, the process of compensating the water and electrolyte balance becomes much more complicated; in this case, the development of shock is typical (see the full body of knowledge) with a significant decrease in the volume of circulating plasma, a sharp violation of microcirculation (see the full body of knowledge), tissue hypoxia (see the full body of knowledge) and decompensated metabolic acidosis (see the full body of knowledge). In the absence of adequate therapy, dehydration and metabolic disorders become irreversible.
The different course of the disease (in some patients - profuse diarrhea with all the consequences mentioned above, in others - the infectious process is limited to the state of vibrio-carrying) cannot be explained only by the influence of cholerogen; apparently great importance has a state of local and general immunity of the patient's body (see the full body of knowledge: Immunity).
pathological anatomy
The morphology of cholera was first described by N. I. Pirogov in 1849. The most distinct morphological signs of the disease are determined in those who died in the algid period. Characterized by a sharp emaciation caused by a rapidly developing dehydration syndrome. Rigor mortis sets in early and quickly (see the full body of knowledge: Post-mortem changes), which persists for 3-4 days. The upper and lower limbs of the corpse are bent, which gives it a peculiar appearance, reminiscent of the pose of a gladiator. During the first hour after the death of the patient, the skeletal muscles can relax and contract, which is accompanied by their twitching. The skin is dry, flabby, wrinkled, especially on the fingers (the washerwoman's hand), sometimes (during the first hours after death) the skin resembles a goose. The skin color is cyanotic with dark purple cadaveric spots. The mucous membrane of the lips is dry, cyanotic, the tip of the nose and auricles are cyanotic. Eyes deeply sunken, half-open, protruding cheekbones, cheeks sunken. The abdomen is drawn in. When opening the corpse of a cholera patient, there is no pungent smell, since putrefaction occurs late. The subcutaneous tissue is dry. Dryness and dark red color of skeletal muscles are characteristic. Serous membranes are dryish with injected vessels, often have a matte tint and pink-yellow (peach) color. On the serous membrane of the intestine, a mucoid, sticky effusion is found, forming thin threads stretching between the loops of the small intestines. The small intestine is flabby, sharply distended with thickened heavy loops. In the lumen of the intestines and stomach contains a large amount of colorless, pinkish or yellowish liquid with a characteristic odor, which looks like rice water. The mucous membrane of the small intestine is pale, with a characteristic absence of bile imbibition. Microscopically, acute serous, rarely serous hemorrhagic enteritis is detected (see full body of knowledge), a sharp plethora of the mucous membrane, edema of the submucosal and muscle layers. With serous-hemorrhagic enteritis, in some places on the surface of the mucous membrane, especially the ileum, there are areas of intense hyperemia with small and larger areas of hemorrhage, a slight swelling of Peyer's patches (group lymphatic, follicles) and solitary lymphatic, follicles, often with a halo of hemorrhages along the periphery. In acute serous enteritis, the mucous membrane of the small intestine is swollen, edematous, full-blooded throughout. In cases where the autopsy was performed shortly after the death of the patient, in smears from the mucous membrane, stained with diluted carbolic fuchsin (see the full body of knowledge), it is possible to detect cholera vibrios.
Edema is expressed in the mucous membrane, submucosal and muscular layers of the small intestine, hemorrhages, lymphoid and plasmacytic infiltration occur. In the cells of the intramural (Meissner and Auerbach) nerve plexuses (see the full body of knowledge: Intestine, anatomy), swelling of the cytoplasm, karyopyknosis, karyolysis, chromatolysis is noted (see the full body of knowledge: Cell nucleus), in some cases, destruction of nerve cells with proliferation of elements of neuroglia is observed - satellites, as well as signs of neuronophagia (see the full body of knowledge).
In the stomach, there is a picture of serous or serous-hemorrhagic gastritis (see full body of knowledge). The gallbladder is distended, with clear, watery bile (white bile) or cloudy contents in its lumen. The mucous membrane of the gallbladder is hyperemic, sometimes with small hemorrhages. In the parenchyma of the liver, dystrophic changes are noted, sometimes areas of focal necrosis, hemosiderosis are found (see the full body of knowledge), hyperplasia of stellate reticuloendotheliocytes (see the full body of knowledge: Liver, pathological anatomy), thrombophlebitis of small, and sometimes large veins (see the full body of knowledge: thrombophlebitis). In cholera, it is also possible to damage the large intestine such as diphtheritic colitis (see full body of knowledge). Inflammatory reactions of the mucous membrane of the pharynx, larynx, bladder, vagina may occur.
The spleen is usually reduced, especially in the algid period, flabby, with a wrinkled capsule. Microscopically, it is often possible to detect plethora, hypoplasia of the lymphatic, follicles, as well as moderately pronounced hemosiderosis.
Changes in the kidneys are more diverse, in which both anemia and plethora can be observed, as well as moderate or severe dystrophic changes in the epithelium, sometimes even necrosis of the epithelium of the convoluted tubules. The permeability of capillaries is increased, as a result, a granular protein mass accumulates in the capsule of the renal glomeruli and in the lumen of the convoluted tubules. The interstitial tissue of the medulla is edematous. The lumens of the straight tubules and collecting ducts are compressed by edematous fluid.
The lungs are dry, collapsed, anemia and dehydration are observed in them, against the background of which foci of bronchopneumonia and edema can be detected. In the interstitial tissue of the lungs, hemosiderin is detected. The cavities of the heart contain dark liquid blood and blood clots. Due to exicosis, the amount of fluid contained in the pericardial cavity decreases, or it is completely absent. The surface of the serous membrane is sticky, more often hemorrhages are found in the epicardium. In the myocardium, protein (granular) and fatty degeneration are noted. In the conducting system of the heart, as well as in the nerve plexuses of the small intestine, there are changes in nerve cells.
In the brain, venous stasis, serous impregnation of the pia mater with diapedesis of erythrocytes, an increase in the amount of fluid in the ventricles, degeneration of nerve cells, neuronophagia (see full body of knowledge), hemorrhages are detected. In the cortex and subcortical nodes, there is perivascular edema with grains and filaments of protein coagulated during fixation. The nerve cells of the brain are swollen, but their pycnosis is also possible (see the full body of knowledge). Hyperchromatosis of individual nuclei is noted, nerve cells with destroyed nuclei and degranulation of Nissl granularity are often found (see the full body of knowledge: Nerve cell).
Damage to the endocrine glands in cholera has not been studied enough. In the adrenal glands, areas with serous impregnation of the stroma are found, and in the cortical substance - zones with cells devoid of lipids. There are signs of decreased neurosecretion in the posterior pituitary gland.
At present, cholera pathomorphosis has been observed everywhere (see the full body of knowledge: Pathomorphosis), due to early hospitalization of patients, timely dehydration therapy, the use of antibiotics and preventive vaccination (see the full body of knowledge: below). In this regard, during the autopsy of a patient who died of cholera, usually no signs of dehydration, pronounced gladiator posture, dryness, flabbiness and wrinkling of the skin of the fingers are found. Indistinctly expressed changes in the intestine, however, hyperemia of the mucous membrane of the small intestine with small hemorrhages, stickiness of the peritoneum and weak signs of enteritis are observed.
In those who died from El Tor cholera with IV degree of dehydration, an autopsy can reveal hyperemia of the gastric mucosa with small punctate and large hemorrhages. The small intestine is distended with a turbid (milky) or colorless liquid, sometimes resembling rice water, or due to the admixture of blood, which looks like meat slops. The serous membrane of the small intestine is hyperemic, the mucous membrane is swollen, pink in color with pinpoint or larger hemorrhages, often surrounding Peyer's patches in the form of corollas. Sometimes the mucous membrane of the small intestine is covered with pityriasis. The mucous membrane of the large intestine is pale. Mesenteric lymph nodes are swollen, hyperplastic. Histological examination reveals superficial gastritis with desquamation of the epithelium. In the mucous membrane of the small intestine, there is an intense desquamation of the epithelium of the villi, especially in their apical sections. At the same time, the epithelium of the basal sections of the crypts was preserved. The number of goblet cells of the mucosal epithelium is increased. Some villi show areas of necrosis. The stroma of the villi is densely infiltrated with lymphocytes and plasma cells; there are few segmented leukocytes. As with other intestinal infections, lesions of the mucous membrane are focal in nature. The results of bacteriological studies are of leading importance in the diagnosis.
Significant changes in the understanding of the pathogenesis and pathomorphology of cholera have occurred as a result of the introduction into medical practice of aspiration biopsy (see full body of knowledge) of the mucous membrane of the gastrointestinal tract. Using this method, Sprinz (Sprinz, 1962), V. I. Pokrovsky and N. B. Shalygina (1972), Fresh (J. W. Fresh, 1974) with coworkers found that the epithelium of the small intestine mucosa not only does not undergo desquamation, but significant damage. In the first days of the disease, enterocytes look swollen, but retain their basic morphological properties. The most characteristic is the stasis and plethora of capillaries, the expansion of the lymphatic, sinuses and blood vessels, a sharp swelling of the basement membranes. Capillary endothelial cells are vacuolated for the most part, basal membranes of vessels and mucosal epithelium are not detected or have the appearance of a wide blurred strip. In the lamina propria, both in the villi and in the area of the crypts, there is a sharp serous edema. The severity of edema and swelling of the basement membranes does not depend on the degree of dehydration of the body, however, it correlates quite clearly with the nature of the bowel movements. So, on the 6-7th day of the disease in patients with semi-formed or formed stools, edema of the mucous membrane of the small intestine is almost completely absent and basement membranes are much more clearly detected; in persons with ongoing diarrhea, the mucous membrane looks almost the same as on the 1st-2nd day of illness.
A biopsy of the gastric mucosa showed an acute catarrhal-exudative or catarrhal-hemorrhagic process with paralytic capillary expansion, plasmorrhagia, edema, and very moderate inflammatory infiltration. There is a sharp vacuolization, and sometimes the death of parietal cells. Swelling of the endothelium of capillaries and basal membranes is as pronounced as in the small intestine. The large intestine is much less affected than the small intestine and stomach. In the first days of the disease, edema and hypersecretion of watered mucus in the sigmoid and rectum were noted.
Vibrio cholerae is found in the small intestine, stomach and large intestine, both in patients with cholera and in vibrio carriers. Most often, it is located in the immediate vicinity of the villi of the mucous membrane, less often in the lumen of the crypts, but is never found inside the tissue. Often, vibrios are detected morphologically in the late stages of the disease (12-20th day), when bacteriological analysis of feces has been repeatedly performed and gave negative results.
The results of aspiration biopsy and changes found in the intestine at autopsy are not always comparable. Aspiration biopsy makes it possible to obtain for examination only sections of the tissue of the mucous membrane of the initial sections of the gastrointestinal tract (stomach, duodenum), therefore, due, as a rule, to a focal lesion of the small intestine in cholera, the material can be taken from an unaffected area. In this regard, based on the data of aspiration biopsy, there is no reason to speak about the absence of inflammation in the entire gastrointestinal tract in cholera.
Clinical picture
Most clinicians [M. I. Afanasiev and P. B. Vaks; S. I. Zlatogorov, N. K. Rozenberg, G. P. Rudnev, I. K. Musabaev, R. L. Pollitzer and others] singled out various clinical, forms and variants of the course of cholera, however, the classifications they proposed did not adequately reflect the leading link in the pathogenesis of the disease is the degree of dehydration (dehydration) of the patient's body, which determines the clinical manifestations of the disease, its outcome and treatment tactics. As mentioned above, there are clinical course of cholera with dehydration of I, II, III and IV degrees and vibrio carrying. The clinical course of classical cholera and El Tor cholera is similar, although it has some features (see the full body of knowledge: below).
The incubation period ranges from several hours to 5 days, more often 2-3 days. It is shorter in persons with chronic diseases of the gastrointestinal tract, especially with achlorhydria (see full body of knowledge) and after gastric resection. In vaccinated, it can be extended up to 9-10 days. The disease often begins with a prodromal period in the form of malaise, weakness, dizziness, slight chills, sometimes fever up to 37-38 °. The first clinical sign of cholera is diarrhea, which begins mainly at night or in the morning; if the disease progresses, then vomiting joins the frequent stool.
Cholera patients with grade I dehydration usually have a gradual onset of symptoms. In almost 1/3 of cases, feces are mushy in nature. Chair usually up to 3 times a day. However, even when its frequency reaches 10 times a day, bowel movements are not plentiful. Accession of vomiting is observed in less than half of the patients; it usually occurs up to 3 times a day. Initial fluid loss does not exceed 3% of the patient's body weight. As a result, the symptoms of dehydration and hemodynamic disturbances are not very pronounced (see the full body of knowledge: Dehydration of the body). A similar mild course of cholera is currently observed in more than half of the patients.
In cholera with dehydration of the II degree, an acute onset of the disease is characteristic; only in a small proportion of patients prodromal phenomena are possible. The stools quickly become watery and in half of the patients resemble rice water - a cloudy white liquid with floating flakes, the stools have no smell. Stool - from 3 to 20 or more times a day. With each bowel movement, 300-500 milliliters of bowel movements (sometimes up to 1 liter) can be released. Defecation is painless. At the same time, there is profuse vomiting, often a fountain. Sometimes vomiting precedes diarrhea. Characterized by the suddenness of vomiting, the absence of previous nausea. Initially, the vomit may contain food debris, an admixture of bile, but very soon they become watery and also resemble rice water in appearance. The addition of vomiting further accelerates the development of dehydration; fluid loss reaches 4-6% of body weight. Patients feel increasing muscle weakness, pain and convulsive twitches in the calf and masticatory muscles. Often there is dizziness, fainting. Patients are pale, acrocyanosis may be observed (see full body of knowledge), mucous membranes are dry. Due to the dryness of the mucous membrane of the larynx and pharynx, the voice is weakened, in some patients it is hoarse. In some patients, there is a decrease in skin turgor, especially on the hands, tachycardia (see the full body of knowledge), moderate hypotension (see the full body of knowledge: Arterial hypotension), oliguria (see the full body of knowledge).
In patients with dehydration of the III degree, abundant watery stools are observed (in some cases, the number of bowel movements cannot be counted) and vomiting (in 1/3 of patients - up to 15-20 times a day). Fluid loss is 7-9% of the patient's body weight. Weakness develops rapidly, often giving way to adynamia (see full body of knowledge). Patients are worried about unquenchable thirst, often they become excited, irritable, complain of pulling pains and cramps in the muscles, more often the calf. Body temperature, which at the beginning of the disease could be elevated, progressively decreases and in almost 1/3 of patients reaches subnormal numbers. Facial features are sharpened, eyeballs sink, often the eyes are surrounded by circles of cyanotic color (a symptom of dark glasses). In most patients, there is a decrease in skin turgor, mainly on the extremities, often wrinkling and wrinkling of it. Pronounced dryness of the skin and mucous membranes, acrocyanosis. For most patients, speech in a whisper, hoarseness and hoarseness of voice are characteristic. Tachycardia is noted. weakening of the pulse, severe hypotension, oliguria.
Cholera with IV degree dehydration is the most severe form of the disease, which is commonly referred to as algid due to a decrease in body temperature. It was generally accepted that algid develops only after more or less prolonged enteritis and gastroenteritis. However, during epidemics of El Tor cholera, decompensated dehydration in some patients developed rapidly within the first 2-3 hours, and in most within 12 hours. illness. Therefore, after a few hours from the onset of the disease, repeated abundant watery stools and vomiting may stop. Fluid loss is 10% or more of the patient's body weight. In the foreground are hemodynamic disturbances (see the complete body of knowledge) and dehydration phenomena. The skin is cold to the touch and covered with sticky sweat, acrocyanosis is noted, in some patients there is a general cyanosis with a violet-gray color. The skin loses elasticity, wrinkled. Especially characteristic is the wrinkling of the hands - the hands of the laundress. The skin gathered in a fold sometimes does not straighten out within an hour. The patient's face is haggard, his features are pointed, his eyes are sunken, a symptom of dark glasses appears, an expression of suffering (facies cholerica). Muscle cramps are prolonged; periods of relaxation may not be expressed and therefore the limbs take a forced position. With cramps of the fingers and hands, a spasm is observed in the form of an obstetrician's hand. There may be a convulsive contraction of the muscles of the abdominal wall, which leads to pain, clonic convulsions of the diaphragm cause painful hiccups. Most patients do not have a pulse. Heart sounds are barely heard, heart contractions are very frequent, arrhythmic. Breathing speeded up, then becomes superficial, arrhythmic. Patients experience a feeling of suffocation. Flatulence is often noted (see full body of knowledge) as a result of intestinal paresis; oliguria, turning into anuria. The body temperature in the armpits is below 36°. Consciousness in patients with cholera remains clear for a long time. Soporous state (see Stunning) or even cholera chlorhydropenic coma (see full body of knowledge) develop only shortly before death and are due to the accumulation of a large amount of under-oxidized metabolic products in the body and a sharp decrease in the antitoxic function of the liver.
Sometimes in patients with cholera with IV degree dehydration, a fulminant course of the disease is observed with a sudden onset, rapid development of dehydration (maybe in the first 1-4 hours from the moment of the disease), with signs of meningoencephalitis.
A feature of the course of El Tor cholera is a greater variety of clinical manifestations: a more frequent course of the disease with dehydration of I - II degrees and in the form of vibrio carriers; more often there is an increase in temperature, almost half of the patients have aching pains in the abdomen, pain in the epigastrium or in the umbilical region.
In previous epidemics, the so-called dry cholera was recorded, which proceeded without diarrhea and vomiting. A similar course of the disease was more common in emaciated individuals and usually ended in death within a few hours with symptoms of cardiopulmonary insufficiency. The absence of diarrhea and vomiting in this case, apparently, is due to early onset paresis of the smooth muscles of the gastrointestinal tract.
In the foci of cholera, asymptomatic vibrio carrying is detected when the pathogen is released, and especially often in persons who have been in contact with cholera patients. V. I. Pokrovsky, V. V. Maleev (1978) believe that the detection of histomorphological and immunological changes in the body in vibrio carriers during an appropriate examination indicates a subclinical course of the infectious process, which is also observed with the bacteriocarrier of other pathogenic microbes of the intestinal group.
Diagnosis
The diagnosis is established on the basis of epidemiological history data (for example, contact with cholera patients, the use of non-disinfected water from open reservoirs), clinical pictures, and laboratory results.
Blood changes are primarily associated with dehydration. With dehydration of the 1st degree, the changes are very moderate: a decrease in the number of erythrocytes and hemoglobin content while maintaining a constant color index, ROE is moderately accelerated, leukocytosis or leukopenia are possible. With dehydration of the II degree, leukocytosis is observed 2½ times more often and reaches 10-103 and more per 1 microliter of blood. With dehydration III-IV degree, the content of hemoglobin and erythrocytes is also, as a rule, reduced. Leukocytosis is observed more often and reaches 15-103-20-103 in 1 microliter. An increase in the number of leukocytes occurs due to neutrophils, with relative monocytopenia, lymphocytopenia and aneosinophilia. A shift in the blood formula to the left is characteristic.
With the initial degrees of dehydration (I and II degrees), blood clotting is usually absent; on the contrary, in some patients, compensatory hemodilution is observed - the relative density and viscosity of the blood are somewhat reduced (1.0225 - 1.0217 grams / milliliters and 4.0, respectively). In a significant proportion of patients with grade III dehydration, relative blood density, hematocrit index, and blood viscosity are also at the upper limit of normal; with IV degree dehydration, blood clotting is the most characteristic sign (plasma density reaches 1.045-1.050 grams / milliliters, hematocrit index and blood viscosity are 60.0-70.0 and 9.0-10.0, respectively). The electrolyte composition of the blood during dehydration I and II degree changes relatively little. In patients with grade III dehydration, electrolyte disturbances are significant - hypokalemia and hypochloremia are pronounced. In grade IV dehydration, in addition to a decrease in the content of potassium and chlorine in the blood, there is a significant deficiency of bicarbonate, decompensated metabolic acidosis (see the full body of knowledge) and respiratory alkalosis (see the full body of knowledge), hypoxia (see the full body of knowledge) and acceleration of I and II phases of blood coagulation with increased fibrinolysis (see the full body of knowledge) and thrombocytopenia (see the full body of knowledge).
The final diagnosis is made on the basis of the results of bacteriological studies.
Laboratory diagnostics. Apply bacteriological and serological methods of research and detection of a specific bacteriophage.
The bacteriological method is the main one and serves to diagnose the disease and identify the pathogen in environmental objects. It is based on the isolation of a pure culture of the pathogen (see the full body of knowledge: Bacteriological methods) and its identification (see the full body of knowledge: Identification of microbes). The selection of culture is carried out in stages. The study involves sowing feces, vomit, bile and others on liquid low-nutrient alkaline media (pH 8.0-8.2), such as 1% peptone water or 1% peptone water with potassium tellurite for the accumulation of cholera vibrios, followed by sowing on dense nutrient media (see the full body of knowledge). Such accumulation is performed twice (I and II accumulation media). In parallel, the native material is inoculated on dense nutrient media - simple (Hottinger agar, meat-peptone, pH 7.8-8.6) and elective (ACDS - agar colored differential medium and others). Crops are incubated at t° 37° in 1% peptone water for 6-8 hours, on alkaline agar - 12-14 hours, in 1% peptone water with potassium tellurite - 16-18 hours and on dense elective media - 18-24 hours .
As they grow from the accumulation media, seedings are made on dense nutrient media, and in case of suspicion of the presence of cholera vibrios, microscopy of smears, the study of mobility and the approximate agglutination reaction on glass with cholera sera (see the full body of knowledge: Agglutination). Suspicious colonies are selected on dense nutrient media, with the material from them they are tested for oxidase (see the full body of knowledge: Oxidase reactions), and the rest of the colony is screened for polycarbohydrate media. If cholera is suspected with material from the colonies, an approximate agglutination test is performed with cholera serum 01 and sera of Ogawa and Inaba. The material from agglutinating colonies is sifted onto polycarbohydrate and ordinary agar media, from non-agglutinating ones - only into polycarbohydrate ones. On polycarbohydrate media, cultures are selected that cause changes characteristic of vibrios. With the help of identifying tests (see the full body of knowledge: section Etiology), the genus, species, biovar and serotype (serovar) of pure cultures obtained at various stages of the study are determined.
To obtain a positive response, an abbreviated identification is sufficient, including a detailed agglutination reaction with cholera serum 01 and sera of Ogawa and Inaba, as well as testing for lysis with phage C and El Tor and determination of the Heiberg group. The study takes 18-48 hours, in some cases - up to 72 hours. In a detailed study of the isolated culture, in addition to establishing the species, biovar and serotype, the phage type, virulent and pathogenic properties are determined. To differentiate virulent and avirulent strains, sensitivity to cholera phages is detected and the hemolytic properties of the pathogen are checked.
Serological research methods are additional and make it possible to identify those who have been ill, as well as to judge the intensity of immunity in vaccinated individuals by determining antibodies in serum or blood plasma and in stool filtrate. For this, the reaction for the determination of agglutinins, vibriocidal antibodies and antitoxins is used. In addition to the generally accepted formulation of these reactions, vibriocidal antibodies are determined in blood serum based on the fermentation of carbohydrates, a method is used for the rapid determination of agglutinins in blood serum using a phase-contrast microscope (see the full body of knowledge: Phase-contrast microscopy)), a method for detecting antibodies in blood serum with the help of antigen neutralization reaction (see the complete body of knowledge: Serological studies). The method of enzyme-labeled antibodies is also promising (see the full body of knowledge: Enzyme-immunological method).
Of the accelerated methods of laboratory diagnosis of cholera, the luminescent-serological method is most widely used (see the full body of knowledge: Immunofluorescence) and the reaction of indirect hemagglutination - PHGA (see the full body of knowledge: Hemagglutination). The method of immobilization of vibrios with cholera O-serum, the agglutination reaction using a phase-contrast microscope, the agglutination reaction in peptone water with cholera O-serum, and the phage adsorption reaction (RAF) are also used. All these methods are additional to the main bacteriological method.
An indirect method for diagnosing cholera is the isolation of a specific bacteriophage (see the full body of knowledge: Phage diagnostics). To detect the phage, the test material and a young broth culture of Vibrio cholerae are introduced into the liquid nutrient medium. After incubation at t° 37° for 6-8 hours. filtration is carried out through membrane filters No. 1 or No. 2, and the presence of phage in the filtrate is determined by the Gracia method (see the full body of knowledge: Gracia method).
differential diagnosis. At present, distinguishing cholera from other acute intestinal infections is difficult, especially at the beginning of an outbreak, as it often occurs in a mild form (cholera with grade I dehydration). The greatest difficulty is the differential diagnosis with food toxic infections (see the full body of knowledge: Food toxic infections) and salmonellosis (see the full body of knowledge). These diseases, unlike cholera, often begin with severe chills, are accompanied by high temperature body, abdominal pain, nausea, vomiting, diarrhea joins later. The stool is copious, but retains a fecal character. has a strong fetid odor. Particularly difficult is the differential diagnosis with a rare gastroenteric form of salmonellosis, which occurs with severe dehydration. In some cases, it is impossible to clarify the diagnosis without laboratory data. Cholera must be differentiated from dysentery (see full body of knowledge), which is characterized by pain in the abdomen, scanty stools with an admixture of mucus and blood, tenesmus, false urge to defecate, fever, no signs of dehydration and thickening of the blood. However, in patients with dysentery caused by Shigella Grigoriev-Shiga, severe dehydration and convulsions are possible. According to the clinical course, it resembles cholera with dehydration of I-II degree rotavirus gastroenteritis (see full body of knowledge), it occurs in the form of epidemic outbreaks and is more often observed in autumn-winter. Feces in rotavirus gastroenteritis are watery, frothy, characterized by rough rumbling in the intestines, general weakness, hyperemia and granularity of the pharyngeal mucosa, sometimes hemorrhages.
Cholera should be differentiated from poisoning with poisonous mushrooms (see the full body of knowledge: Mushrooms, v. 29, additional materials), organic and inorganic chemicals or pesticides, with special attention to the history. In case of poisoning, the first clinical signs are nausea, vomiting, severe pain in the abdomen, diarrhea joins later, in the feces there is often an admixture of blood. Body temperature, as a rule, remains normal (see the full body of knowledge: Poisoning).
Treatment
Treatment is most effective in the first hours of the onset of the disease. Therefore, the medical service and, first of all, infectious diseases hospitals, must be in constant readiness to receive cholera patients and have the necessary supply of medicines.
Treatment is determined by the patient's condition, primarily the degree of dehydration. Patients with dehydration I and II, and sometimes III degree, it is usually sufficient to introduce liquid through the mouth. It is best for the patient to drink or inject through a thin tube into the stomach in small portions Oralit liquid containing 3.5 grams of sodium chloride, 2.5 grams of sodium bicarbonate, 1.5 grams of potassium chloride and 20 grams of glucose (sucrose) in 1 liter of water. The volume of fluid drunk should be equal to the volume of fluid lost during the illness by the body with feces, vomit and urine, which is determined by the degree of dehydration. At the same time, there is a rapid disappearance of symptoms of dehydration, restoration of hemodynamics and kidney function. If, with the introduction of liquid into the stomach, the therapeutic effect is insufficient, as well as in cases of dehydration of the III-IV degree, a solution of quartasol or trisol is administered within 2 hours to compensate for existing fluid losses in a volume corresponding to the loss of body weight. Quartasol contains 4.75 grams of sodium chloride, 1.5 grams of potassium chloride, 2.6 grams of sodium acetate and 1 gram of sodium bicarbonate in 1 liter of pyrogen-free water. Trisol, or a 5:4:1 solution, which has received wide international recognition, contains 5 grams of sodium chloride, 4 grams of sodium bicarbonate and 1 gram of potassium chloride in 1 liter of pyrogen-free water. Solutions are administered intravenously or intraarterially. Before the introduction, they should be heated to t ° 38-40 °. The first 2-3 liters are infused at a rate of 100-120 milliliters per 1 minute, then the perfusion rate is gradually reduced to 30-60 milliliters per 1 minute.
Subsequently, ongoing losses of fluid and electrolytes are corrected. In order to more accurately account for losses, a scale-bed or the so-called cholera bed is used. During this period, the volume and speed of fluid administered depend on the frequency of stools, the volume of bowel movements and the amount of vomit: the more the body loses fluid, the more intensively it should be administered. Therefore, every 2 hours, the volume of fluid lost is calculated and the rate of administration of the solution is changed accordingly. For example, if the patient has lost 2.5 liters in the previous 2 hours, then 2.5 liters of solution are injected.
The introduction of a saline solution continues until the diarrhea stops and the kidney function is fully restored, which, on average, for patients with II and III degrees of dehydration is 25-30 hours. Patients with IV degree of dehydration (algid) saline solution is administered most often within 2-4 days. On average, during this time they receive about 36 liters of fluid. The predominance of the amount of urine over the amount of bowel movements allows us to predict the time of stool normalization in 6-12 hours. and stop intravenous fluids in the absence of vomiting. It should be remembered that an adult patient loses 1-1.5 liters of fluid per day through the lungs and skin, this must also be taken into account when compensating for its daily losses.
In children and the elderly, forced fluid administration can cause hyperhydration (excessive fluid content) with the possible development of cerebral and pulmonary edema (see the full body of knowledge: Pulmonary edema, Edema and swelling of the brain), therefore, intravenous infusions in them during primary rehydration spend more slowly (over 3-4 hours or more).
In the period of convalescence, potassium salts are prescribed, more often in the form of a solution consisting of 100 grams of potassium acetate, 100 grams of potassium bicarbonate and 100 grams of potassium citrate in 1 liter of water. This solution patients drink 100 milliliters 3 times a day.
The patient must be carefully cared for. During vomiting, it is necessary to support the patient's head. The disease of cholera is accompanied by a significant decrease in body temperature, therefore, it is necessary to take all measures to warm the patient, it should be warm in the wards. After stopping vomiting, the diet should consist of mucous soups, liquid cereals, yogurt, mashed potatoes, jelly; prescribed vitamins.
All patients and vibrion carriers are prescribed tetracycline 0.3-0.5 grams every 6 hours for 5 days. Smaller single and daily doses delay recovery and lengthen the time for isolating V. cholerae. If patients are intolerant to tetracycline, levomycetin or furazolidone can be used.
Cholera patients are discharged from the hospital after the disappearance of all clinical symptoms and the negative results of three bacteriological studies of feces. Bacteriological studies are carried out 24-36 hours after the end of antibiotic treatment for 3 consecutive days. The first collection of feces is carried out after the appointment of a convalescent saline laxative (20-30 grams of magnesium sulfate). Bacteriological examination of duodenal contents is performed once.
Prevention
Epidemic well-being in cholera can be achieved through the implementation of administrative, communal and medical measures. To this end, a comprehensive anti-epidemic plan is drawn up and annually adjusted by the ministries of health of the union and autonomous republics, regional, regional, district and city health departments together with departmental health authorities in the republic, territory, region, city and district. The plan is approved by the Councils of Ministers of the Union and Autonomous Republics and by the Territorial, Regional, City and District Executive Committees of the Soviets of People's Deputies. The plan, in particular, provides for: the preparation of appropriate premises and the drawing up of schemes for the deployment of hospitals for cholera patients, provisional hospitals, isolators (see the full body of knowledge), observers (see the full body of knowledge: Observation Point) and bacteriological laboratories (see the full body of knowledge knowledge); creation of a material and technical base for the listed institutions; training of medical workers in epidemiology, laboratory diagnostics, clinic and treatment of cholera (differentiated for different categories of trainees); the alignment of forces available in the region (republic, territory) to ensure, if necessary, treatment-and-prophylactic and anti-epidemic measures. Therapeutic and prophylactic and anti-epidemic measures differ somewhat depending on the epidemic situation: with the threat of the spread of cholera, in the focus of cholera and after the elimination of the focus of cholera.
Measures for the threat of the spread of cholera. A region (oblast, kray) is declared endangered if in the neighboring administrative territory, including neighboring countries, or in the territory of a non-adjacent foreign state with which there are intensive direct transport links, cases of cholera have become widespread. A set of measures to prevent cholera in areas where there is a threat of introducing this disease is carried out according to pre-developed plans, which are adjusted in accordance with the specific epidemic situation.
General management of cholera prevention activities is carried out by emergency anti-epidemic commissions (EPC) of the republic, region (territory), city, district. Under emergency anti-epidemic commissions, a permanent operational body is created - an anti-epidemic headquarters headed by the head of the regional (territorial), city health department or the chief physician of the district.
In the territory where the possibility of introducing cholera is expected, patients with acute gastrointestinal diseases are actively identified and hospitalized in provisional departments with a mandatory single bacteriological examination for cholera; if necessary, vaccination of the population is carried out (see the full body of knowledge: below); persons arriving from places unfavorable for cholera, without certificates of observation (see full body of knowledge) in the outbreak or with an incorrectly issued certificate, are subject to a 5-day observation with a single bacteriological examination for cholera. It is forbidden to sell antibiotics and sulfa drugs without a doctor's prescription. The water of open reservoirs and sources of centralized water supply, as well as household wastewater, are examined for the presence of cholera vibrios. Health authorities and institutions carry out a ten-day analysis of the incidence of acute intestinal infections with their etiological interpretation. Control over the sanitary protection of water sources is being strengthened (see the full body of knowledge: Sanitary protection of water bodies) and the regime of water chlorination (see the full body of knowledge: Chlorination of drinking water); the amount of residual chlorine in the water supply network is brought to 0.3-0.4 milligrams per 1 liter. In settlements that do not have a centralized water supply, it is prohibited to use water for drinking and household purposes from open reservoirs (rivers, canals, lakes) without prior disinfection (see the full body of knowledge: Water disinfection). To provide the population with water, delivery of high-quality tap water is organized. Field camps, educational institutions, enterprises and institutions are provided with chlorinated or freshly boiled water. Control over the sanitary condition of settlements, public catering establishments and the food industry is being strengthened. Particular attention is paid to maintaining proper sanitary condition in crowded places (markets, transport, train stations, campsites, hotels and others) and in public latrines. The fight against flies is carried out, especially in places of their possible breeding. On all highways leading from cholera-affected areas, temporary sanitary checkpoints (SCP) are organized by medical workers, and checkpoints (checkpoints) are organized by police forces. Sanitary checkpoints are also organized at railway, river, sea stations and bus stations, as well as at airports (see the full body of knowledge: Quarantine, quarantine).
Sanitary checkpoints are responsible for identifying patients with gastrointestinal disorders; identifying persons coming from cholera-prone areas and checking whether they have observation certificates. Sanitary control points are also responsible for providing vehicles with disinfectants.
Patients with gastrointestinal disorders identified at sanitary control points are sent to the nearest provisional hospital, and lists are compiled for persons who have been in contact with such patients, coming from cholera-prone areas, which are transferred to the territorial (at the place of residence) SES for monitoring these persons and examining them for vibrio-carrying.
Passenger trains and ships flying from cholera-affected areas are escorted by teams consisting of a medical worker and a police representative. The duties of the brigades accompanying trains and ships include: identifying patients with gastrointestinal disorders and those who were in contact with them, monitoring compliance with the sanitary condition on vehicles, and conducting sanitary and educational work among passengers. A patient with gastrointestinal disorders identified along the route is immediately temporarily isolated in one of the vacated compartments (cabin), material for bacteriological examination (faeces, vomit) is taken from him, and current disinfection is carried out in common areas.
Administrative and medical measures to prevent the introduction of cholera from foreign countries are carried out in accordance with the current International Health Regulations (see the complete body of knowledge) and the Rules for the Sanitary Protection of the USSR Territory from the Importation and Spread of Quarantine and Other Infectious Diseases (see the full body of knowledge: Sanitary area protection).
Activities in the focus of cholera. The focus of cholera is individual households, a residential area (a group of houses), a city district, a settlement, a city or a group of settlements, united by industrial, transport links, proximity to the place where cholera patients or vibrio carriers are found. When diseases (or vibrio-carrying) are detected in a number of settlements, the entire administrative territory of a district, region, or territory can be the source of cholera.
Anti-epidemic and sanitary-preventive measures aimed at localizing and eliminating the focus of cholera are: restrictive measures and quarantine (see the full body of knowledge: Quarantine, quarantine); identification and hospitalization of patients with cholera; identification and hospitalization of patients with acute gastrointestinal diseases; identification and hospitalization of vibrio carriers; identification and isolation of persons in contact with patients, vibrio carriers, as well as those who were in contact with environmental objects, the infection of which has been established; epidemiological examination (see the complete body of knowledge) in each individual case of cholera; bacteriological examination of patients, vibrio carriers, persons in contact with the patient, as well as environmental objects; treatment of patients with cholera and vibrio carriers; current and final disinfection (see full body of knowledge); cleaning of populated areas (see the full body of knowledge), supply of high-quality water, sanitary and hygienic regime at food industry enterprises, catering and trade facilities; sanitary and educational work among the population.
Activities after the elimination of the focus of cholera. For persons who have had cholera and vibrio carriers, after their sanitation, dispensary observation is established for a period determined by orders of the USSR Ministry of Health. The chief doctor of the hospital informs the head of the regional (city) health department at the place of residence of the discharged person about the discharge of a person who has had cholera or a vibrio carrier (at the end of his sanitation). Dispensary observation is carried out by the office of infectious diseases (see the full body of knowledge). Employees of head water supply facilities, dairy industry, dairy and cheese factories, farms, drain points and the like, workers in the production, processing, storage, procurement, transportation and sale of food and beverages, workers in cleaning and washing production equipment, inventory and containers at food enterprises, all employees of public catering enterprises, persons serving sanatoriums, medical-prof. and children's institutions, are discharged to work after a five-time daily bacteriological examination for vibrio-carrying. Bacteriological examination of persons of these categories before their release to work begins 36 hours after the termination of antibiotic treatment.
In the process of dispensary observation, special attention is paid to bacteriological examination of the sick person. In the first month, a bacteriological study of feces is carried out once every 10 days and once - bile, in the subsequent period, feces are examined once a month. Cholera survivors and sanitized vibrio carriers are removed from dispensary observation after a negative bacteriological examination of feces for cholera. Removal from dispensary registration is carried out by a commission composed of Ch. polyclinic doctor, infectious disease specialist, district doctor and district epidemiologist.
Within a year after the elimination of the cholera outbreak, active identification of patients with acute gastrointestinal disorders is carried out at all stages of providing medical care to the population, as well as by conducting door-to-door rounds once every 5-7 days. Identified patients are immediately hospitalized regardless of the severity and clinical manifestations of the disease. All hospitalized patients are subjected to a three-time (3 consecutive days) examination for vibrio-carrying, vibrocidal antibody titers are determined in paired blood sera. Treatment with antibiotics and sulfa drugs in these patients can be started after the diagnosis of the disease is established.
At least once every 10 days, taking into account the epidemic situation and the sanitary and hygienic condition of the settlement, bacteriological studies of water from sources of drinking water supply, open reservoirs, domestic wastewater for the presence of cholera vibrios are carried out. The amount of residual chlorine in the distributing water supply network is systematically maintained at the level of 0.3-0.4 milligrams/liters.
There is constant strict control over the observance of the sanitary and hygienic regime at public catering enterprises, the food industry and the food trade. Strict constant control is exercised over the timely and high-quality cleaning of settlements, over the correct maintenance of landfills. There is a regular fight against flies. Sanitary clearance is systematically carried out. work (lectures, conversations, speeches in the local press, on radio, television, publication of leaflets, leaflets, etc.) on the prevention of cholera and other gastrointestinal infectious diseases. Vaccination (revaccination) against cholera of the entire population of this territory is carried out.
All of the above activities are carried out within 1 year after the elimination of the cholera outbreak until the end of the next epidemic season, provided that no new cases of diseases or vibrio carriers are detected during this year.
specific prophylaxis. The issue of preventive immunization (see the full body of knowledge) of various contingents and population groups is decided in each specific case, depending on the epidemic situation.
Prophylactic immunization with corpuscular vaccines (see the full body of knowledge: Vaccines) prevents clinically pronounced cholera diseases in approximately 40-50% of vaccinated people for an average of 5-6 months. At the same time, the indicated degree and duration of the effect of prophylactic immunization are observed only after two subcutaneous injections of the vaccine with 7 - 10-day interval; after a single subcutaneous injection of the vaccine, the intensity and duration of the emerging immunity are much less pronounced.
The WHO Committee on International Epidemiological Surveillance of Infectious Diseases in December 1970 stated that at present, vaccination is not an effective method of preventing the spread of cholera, this is confirmed by the fact that in the group of vaccinated patients the incidence rate decreased by about 50% compared to unvaccinated, however, the effect of the vaccine lasted at most 6 months. Moreover, it was found that under normal conditions (i.e., not in the framework of special experiments), vaccination does not give even this degree of reduction in the incidence of cholera for the population of the country as a whole.
When deciding on the advisability of conducting mass cholera vaccinations in the event of a cholera epidemic, it is necessary to take into account the availability of forces and means for hospitalization of all patients, isolation of those who were in contact with them, active identification and hospitalization of all persons suffering from bowel dysfunction, as well as isolation of persons who were with them in contact, laboratory examination of all foci, that is, to carry out activities that should ensure the localization and elimination of the outbreak that has arisen as soon as possible.
Conducting vaccinations in a short time to a large number of people (taking into account the subcutaneous administration of the cholera vaccine) will require a huge amount of medical staff. At the same time, it should be borne in mind that post-vaccination immunity in some of the vaccinated occurs no earlier than the 20th day from the start of immunization; during this time, the epidemic focus can be eliminated with the help of other anti-cholera measures.
Based on the data presented in our country, it was recognized as inappropriate to use cholera vaccination as a measure that can localize and eliminate emerging cholera outbreaks in a short time. The experience of the Soviet Union in eliminating a cholera outbreak without mass vaccination on the basis of epidemiologically sound measures was approved by the WHO Expert Committee (1970), which noted that this experience should serve as an example for other countries facing identical problems.
Mass anti-cholera immunization of the population is fully justified only in cases where a possible cholera epidemic is foreseen or in territories bordering cholera-prone areas and countries where anti-epidemic measures are not carried out actively enough. It is more needed in settlements with unsatisfactory sanitary and communal conditions, where there is an increased incidence of intestinal infections, which indicates the possibility of developing a cholera epidemic in them. In settlements with good sanitary and communal conditions, provided with good-quality drinking water and effective sewage treatment facilities, it is hardly advisable to introduce a system of cholera immunoprophylaxis.
If there are indications for immunoprophylaxis, first of all, vaccinations are given to employees of the public catering network, persons involved in the production, storage, transportation and sale of food, personnel of head water supply facilities and others.
Along with the usual corpuscular vaccine, in recent years a new vaccine has been developed in the USSR - cholerogen toxoid. A comprehensive study of this vaccine has shown that it has an immunogenic advantage over the corpuscular vaccine and weakly expressed reactogenicity, however, the epidemiological effectiveness of the vaccine is still unknown, since it can only be established in a controlled trial carried out under the conditions of the spread of cholera in a certain area. Cholerogen-anatoxin is injected subcutaneously once a year, with revaccination (according to epidemic indications) - no earlier than 3 months after the initial application. For adults (18 years and older), the dose of the drug for primary vaccination and revaccination is 0.5 milliliters, for children aged 15-17 years - 0.3 and 0.5 milliliters, at the age of 11-14 years - 0.2 and 0.4 milliliters, at the age of 7-10 years - 0.1 and 0.2 milliliters.
⇓ Complete body of knowledge. Volume one A. ⇓Cholestasis ⇒
Are you categorically not satisfied with the prospect of irretrievably disappearing from this world? You do not want to end your life path in the form of a disgusting rotting organic mass devoured by grave worms swarming in it? Do you want to return to your youth to live another life? Start all over again? Fix the mistakes you've made? Fulfill unfulfilled dreams? Follow this link:
Everyone who stands out from the masses should be specially noted, each of those who are ready to sacrifice themselves, the great heroes and martyrs who made experiments on themselves. Forgetting about them, the history of medicine, the history of mankind in general, would act unfairly. It is difficult to say who and when was the first. One thing is clear: the history of the heroism of doctors will never end. In the center of a cohort of these people is one of the most famous doctors - Max Pettenkofer. With a story about his feat, we can begin our story.
This is not the doctor's first experience with himself, and if we appreciate Pettenkofer's heroic deed so highly, this is due to the special historical circumstances of that time, as well as the importance of the problem raised. The experiment was carried out on October 7, 1892 by 73-year-old hygienist professor Max Pettenkofer, who, in order to prove the correctness of the theory he defended, drank a culture of cholera vibrios in front of witnesses. The result of this experiment, bordering on almost self-destruction, was downright surprising: Pettenkofer did not contract cholera.
In those days, cholera had long been known in Europe and terrified. Until the first quarter of the 19th century, it was believed that cholera was an epidemic disease, common only in distant countries, and, therefore, there was nothing to be afraid of in Europe. This opinion changed after an epidemic of Asiatic cholera suddenly broke out in India for unknown reasons in 1817, starting from there on its way to the West. Two years later, the epidemic for the first time in history swept Africa, where it was brought by caravaners, and at about the same time penetrated through China to the European part of Russia, first to Orenburg, where it immediately unexpectedly took on an epidemic form, remarkable not so much for the number of deaths. how much mass morbidity. The fury of the epidemic was tamed by a long, cold winter. But in Odessa, cholera was able to deploy all its forces. About half of all patients died there. These statistics are in complete agreement with those obtained in the first world war during the cholera epidemic in the Przemysl fortress.
When an epidemic broke out in Odessa, which broke out at a time still very distant from the era of bacteriology, they tried to prevent the spread of infection with the help of cordons. But it didn't go beyond trying. In 1830, cholera reached Moscow, where, however, only a small number of residents were sick with it. The situation was different in Germany. There, cholera spread a few months later. In August 1831, the first deaths from cholera were recorded in Berlin, then it was the turn of Hamburg. However, some areas of Germany remained unaffected by the epidemic. Cholera, so to speak, jumped over them, infiltrating France and England, from where it was then brought to North America. Transport conditions of that time determined the relatively slow spread of cholera.
First in one place, then in another, small pockets of infection were still observed, but, finally, the epidemic stopped. However, in 1892 a large epidemic of cholera broke out again in Germany, namely in Hamburg, where 18 thousand people fell ill in 5 months, of which 8 thousand died. At that time, the causative agent of cholera was already known. In 1883, Robert Koch discovered the cholera vibrio, shaped like a comma and therefore called the "cholera comma". Toward the autumn of that year, cholera appeared in Egypt; moreover, there was a fear that, as before, she would start her wanderings around the world from there. Therefore, some governments, primarily the French, decided to send research teams to Egypt in order to start studying and combating the epidemic with the help of new methods.

A similar decision was made in Germany. The government appointed Koch head of the commission, which arrived in Alexandria on 24 August. The Greek hospital was chosen as the place of work. A year earlier, Koch had observed a large number of bacteria in a part of the intestine of a cholera deceased sent to him from India. However, he did not attach much importance to this, since there are always a lot of bacteria in the intestines.
Now, in Egypt, he remembered this discovery. "Perhaps," he thought, "it is this microbe that is the desired causative agent of cholera." On September 17, Koch reported to Berlin that a microbe common to this disease had been found in the contents of the intestines of twelve cholera patients and ten who died of cholera and its culture had been grown. But he failed to cause cholera disease by injecting this culture into animals. By this time, the epidemic in Egypt had already begun to subside, and further research seemed impossible. Therefore, the commission went to India, to Calcutta, where cholera was still nesting. The sick and the dead were again subjected to research, and again the same microbe was found as in Egypt - the same comma-shaped bacilli connected in pairs. Koch and his collaborators did not have the slightest doubt that this particular microbe was the causative agent of cholera. Having additionally studied the process of cholera infection and the importance of drinking water supply for stopping the disease, Koch returned to his homeland, where a triumphant meeting awaited him.
Koch was convinced that he had found the causative agent of cholera. Not all researchers shared this point of view, in any case, not all accepted it unconditionally. Pettenkofer also belonged to them. It is worth saying a few words about this man who can be called the founder of modern hygiene and who played an unforgettable role in the history of cholera. He deserves it.
Max Pettenkofer is a man of peculiar destiny. He was the son of a peasant, one of eight children in the family. His father, burdened with worries, was delighted when a childless brother, a court apothecary in Munich, took his sons and took care of them. As it seemed to his uncle, Max would not cause him much trouble. Studying at the gymnasium was easy for the boy. From him, my uncle thought, in time a real apothecary might come out, maybe even his successor. But somehow Max, who at that time was taking a course in a pharmacy and had already risen to the assistant pharmacist, dropped and broke one of the vessels. The angry uncle rewarded the clumsy nephew with a crack, and the latter did not hesitate for a long time. He left his uncle and his pharmacy and went to Augsburg with the intention of becoming an actor.
From Pettenkofer, he became "Tenkof", thus taking the middle part of his last name as a pseudonym. Having played one of the roles in Goethe's "Egmont", he showed the Augsburgers that a new star was about to rise in the theatrical horizon of their city. At least that's what Max thought. But the audience thought differently, and the critics were frankly unfriendly. Nevertheless, Mr. Tenkof continued to persist, although his parents begged him to return to his former profession. He relented only after the intervention of his cousin Elena (secretly from everyone she was his bride), who begged him to become a "decent person" again and continue his teaching. Only my uncle could not reconcile, believing that a man who once became an actor is not able to ever head the court pharmacy. "Such a person is suitable at best for medicine," the good uncle reasoned, and we should be grateful to him for the decision.
Pettenkofer became a physician. He was not attracted to practical medicine, in particular to medical practice. At the same time, as a student, he showed himself capable of medical chemistry, an experimenter, one might even say - a researcher.
Pettenkofer went to Giessen to Liebig, the best chemist of that time, finished his education there and finally entered, for lack of anything better and under pressure from Helen, to serve in the Mint of Munich, although this was not an easy task for him, since he was still a doctor, although by that time he had created a name for himself as a chemist.
Pettenkofer never liked to work systematically. He clutched at one topic, then another, finding in each of them genuine golden grains. This was both in his student years and during his service at the mint. So, he extracted minimal amounts of precious platinum from silver thalers and opened the mystery of antique purple glass. Not surprisingly, his talent was soon noticed: he was appointed professor of medicinal chemistry.
Since then, he has been working at a new place, first on one problem, then on another. He discovered a method for preparing cement, which is not inferior in quality to English, suggested how it is possible to obtain lighting gas not only from expensive coal, but also from cheap wood containing a lot of resin. The failure that befell him was only an episode. In Basel, where his method was put into practice, and where a festival of illumination of the city was solemnly celebrated with the wide participation of the population, the new system failed at the first attempt. Pettenkofer, who was present, felt deeply unhappy. Tears of anger and shame streamed down his cheeks. However, immediately after that, he rushed to Munich, to his laboratory, eager to find the mistake that caused the failure. After two days of work and reflection, the error was found, eliminated, and gas lighting broke out in Basel.
All these events in the life of Pettenkofer were big and important. However, his main merit is that he founded modern hygiene. Random circumstances prompted him, a chemist and technician by profession, to take up hygiene issues.
Somehow he was ordered to find out why the air in the royal castle is so dry that the king constantly feels a tickle in his throat. So, it all started with home hygiene. Then followed clothing hygiene, nutrition, water supply, that is, everything related to the field of public and individual hygiene. The logical conclusion of these studies of Pettenkofer was the creation for him of a special scientific institute - the House of Hygiene, whose activities brought great benefits to the country and the city.
Pettenkofer, of course, also dealt with infectious diseases, since one of the tasks of a hygienist is to prevent the population from diseases. Of all infectious diseases, the scientist was especially interested in cholera, which set him the goals of research and prompted him to create his own theory of the occurrence of this and other epidemic diseases. His interest in cholera is natural, since it was during that period that its epidemics arose especially often. But for him, the study of cholera and the fight against it were not only a stage of research, but, one might say, a personal matter. In this regard, he said: “I fell ill with cholera in 1852, after the epidemic of 1836-1837, when I attended the senior classes of the gymnasium, did not touch me. After me, my cook, who died in the hospital, fell ill, then one of my twin daughters Anna, who recovered with difficulty. These experiences left an indelible mark on my soul and prompted me to explore the ways in which cholera proceeds. We can say that Pettenkofer declared war on cholera.
When Koch discovered Vibrio cholerae, Pettenkofer did not, of course, deny the correctness of this discovery; he himself thought of a stimulus possessing living nature. But he had other ideas about it. First of all, Pettenkofer did not believe in the simple transmission of infection and said: “At present, the question is mainly how to get close to this bacillus, how to destroy it or prevent its spread. The fight against microbes is now considered the only effective prevention and a whole series of epidemiological facts that strongly argue against the hypothesis that cholera is simply contagious. Many people judge more and more by observing the "cholera comma" in a flask, or on a glass plate, or in cultures, completely unconcerned with how cholera looks in the process of practical epidemiological spread ".
Naturally, Pettenkofer approached the problem of cholera primarily from the standpoint of his science. As a professor of hygiene, he even had to lecture on the subject, not to mention the fact that, as said above, he considered cholera almost as his personal enemy.
Even the “microbe hunters,” as Pettenkofer called them, proved by their existence that there are people who, due to the characteristics of their body or for some other reason that protects them from illness, remain healthy even with a strong epidemic. The phenomenon of innate or acquired immunity has long been known. It is also known that in each individual case, the state of human health, in particular the functioning of the stomach and intestines, plays an important role.
For Pettenkofer, the problem of cholera as a whole was an equation, first with two, then even with three unknowns. The discovery of the "cholera comma" did not yet bring clarity to this equation. No doubt he could consider himself an epidemiologist. "There are," he said, "territorial and temporal factors favoring the emergence of an epidemic." In this regard, he attached the greatest importance to the state of groundwater. In his opinion, the process of decay of organic substances with which the carrier of cholera merges depends on the saturation of the soil with water. By the carrier of cholera, he meant a specific substance of extremely small volume with an internal organization, like those that cause fermentation.
Pettenkofer was Munich's hygienist and was responsible for the city's health care. In accordance with his theory, he ordered that the streets of the city be kept clean in order to counteract the development of cholera carriers. Disinfection of the feces and urine of patients, recommended by him at first - a mention of this can be found in documents on cholera dating back to 1866 - he no longer trusted, considering it at best a preventive tool used even before the outbreak. He, of course, spoke out against unreasonable attempts to disinfect letters coming from distant countries (they were first pierced with a needle and then fumigated). He was also opposed to quarantines and recommended that, at the onset of cholera, go to areas recognized as free from infection.
It is not surprising that such opinions and proposals of Pettenkofer caused a sharp protest among many; there were, however, scientists who defended his point of view. Many of them, even Virchow, were impressed by the idea of groundwater.
Pettenkofer constantly traveled to places where material could be found to support his views; for this purpose he spared neither effort nor money. It was not easy for his opponents.
"Why," he asked, "is there cholera in one city and not in another? It's all about the soil."
“Not without trembling, not without fear,” he said, “I present evidence to my judges and I want this evidence to unite everyone in the great struggle for the good of mankind.”
Pettenkofer, like others who doubted that the microbe discovered by Koch caused cholera, had a strong argument. A very important link was missing from the chain of evidence cited by Koch that Vibrio cholerae was the sole culprit in the outbreak of the cholera epidemic.
How was the situation before, when, for example, the causative agent of tetanus was discovered, or when it was said that the microbe of rabies must be in the spinal cord or brain? Then a culture of the appropriate bacteria, or some other substance suspected of being present, was injected into the animal in order to cause the same disease in it. But with cholera it was different.
There were no animal experiments. Koch could not give a single example to prove that the microbe he discovered causes cholera in a healthy animal. He could not do this, because, despite all attempts, not a single animal showed susceptibility to cholera. Cholera is a human disease, and animal experiments failed the researcher. It was the missing link in the chain of evidence, the link that kept the chain open. And then Pettenkofer decided to do something that, of course, no one dared even think about: to conduct an experiment on a person, on himself.
Pettenkofer's historical experience took place on the morning of October 7, 1892, at a time when cases of cholera were multiplying in Hamburg and Paris and the entire population was terrified, and in Munich, despite the large number of visitors (the October holiday was not canceled), cholera outbreaks did not were observed. This circumstance only strengthened Pettenkofer in the opinion that not one microbe, but also the characteristics of the season and soil, or other similar circumstances, determine the occurrence of an epidemic.
The experiment was, of course, carried out in great secrecy. Pettenkofer ordered from the Berlin Institute of Health a culture of cholera bacilli prepared on a well-known gelatinous substance - agar, which is extracted from algae. A broth culture was prepared from this pure culture on agar at the Munich Institute of Hygiene; microbes took root perfectly, quickly multiplied and formed entire colonies in a nutrient medium favorable for them. There were myriads of bacilli in the culture, and even if the culture were diluted a thousand times, there would still be countless "cholera commas" in every cubic centimeter of it.
Pettenkofer later said: "In one cubic centimeter, I apparently took a billion of these fearsome microbes, in any case, much more than when touching the lips with unwashed fingers." However, he did everything not to succumb to self-deception and to get a clear result. "It is very likely," he thought, "that the hydrochloric acid of the gastric juice will damage the microbes so much that they can no longer be the causative agents of the disease." Therefore, he poured a gram of baking soda into one hundred grams of water (about half a tea glass), poured a cubic centimeter of fresh “microbial soup” into it and drank the contents without taking a breath. After that, he poured some more water into the glass and drank it, so as not to miss the microbes remaining on the walls of the glass.
The experiment, as has already been said, was carried out in the morning, but before that Pettenkofer, as usual, had breakfast. After the experience, he continued to lead his usual way of life, eating and drinking, as always, quite a lot. This happened, therefore, on October 7th. Three days later, Pettenkofer fell ill with intestinal catarrh, the symptoms of which seemed to indicate exposure to cholera vibrios. But, despite this, his state of health did not worsen, there was no lack of appetite. At first, Pettenkofer did not see the need to prescribe a diet for himself and change anything in his familiar and beloved simple Munich cuisine. Only when the intestines did not calm down, and on October 13 his condition even worsened, did the scientist change his diet, eating only what was useful in such a state. The very next day his bowels were fine again. All this time, Pettenkofer did not take medication.
Of course, he made a bacteriological examination of the faeces. The analysis showed a large number of cholera vibrios. The watery discharge looked like pure cultures of these bacilli. When on October 14 the intestines calmed down and the discharge became normal again, cholera microbes were already noted in small quantities, and two days later they disappeared completely.
The conclusions drawn by Pettenkofer from experience confirmed the point of view so ardently defended by him, and he, to an even greater extent than before, was imbued with the conviction of the correctness of his views on the origin of the epidemic.
It goes without saying that Pettenkofer's assistants tried to keep him from the heroic experiment. They begged him to subject someone younger to this ordeal, but, knowing Pettenkofer's persistence, they were at the same time convinced that it was impossible to dissuade him from carrying out the once planned plan. When, on October 15, it became clear that Pettenkofer was not a bacillus carrier and his point of view seemed to be confirmed, the fewer objections remained to repeating the experiment, now devoid of the fear that it had caused before. On the other hand, it seemed that the repetition of experience was of great importance. His collaborator Rudolf Emmerich - later Pettenkofer's successor at the department in Munich - decided on this. He was 34 years younger than his teacher and was renowned as a hygienist.
Emmerich conducted his experiment on 17 October. He also prepared a solution of baking soda in water, adding to it one tenth of a cubic centimeter of a daily, luxuriantly developed cholera culture, that is, much less than the amount accepted by Pettenkofer. But Emmerich complicated his experience by the fact that after taking the culture, he deliberately drank and ate more than usual. By worsening the diet, Emmerich thereby wanted to reduce the body's resistance, which played a certain role in Pettenkofer's theory about the factors of cholera.
But Emmerich wanted to further weaken his body in order to create the most favorable opportunities for bacteria to develop. Dressed only in a shirt, he was exposed to a current of cold air, repeating this many times, until he finally felt sick. The catarrh of the intestines that began in him proceeded in a more severe form than that of Pettenkofer, and very soon required medical attention. But it wasn't real cholera. Emmerich felt well, his mood remained good. The persistent feeling of weakness felt in cholera, partly due to microbial poisoning, partly due to large losses of water in the body, did not occur; only the restriction of the diet caused him inconvenience. On October 24, he was already able to return to his usual diet. Vibrios cholerae were noted in his secretions until 28 October.
Was it cholera or not? Pettenkofer and Emmerich disputed that they had cholera. Pettenkofer wrote: “I allow myself to assume that Robert Koch and his numerous followers will say that nothing has been proven, except what they previously assumed, namely, that Emmerich and I, after taking“ cholera commas ”, suffered an outbreak of real cholera, it’s true in a mild form and without a fatal outcome. I am pleased to give my opponents this pleasure, but I still cannot agree with their views. "
It is now known that Pettenkofer was wrong, and Koch was absolutely right. But it is also known that pathogens do not always have the same strength or, as they say, the same virulence. Some of them cause a strong, others, on the contrary, a weak infection. An important role is also played by the body's resistance. Everyone knows this on the basis of their everyday observations. Heroic experiments are not needed to prove this.
Therefore, the experience that Pettenkofer put on himself was undesirable already at that time. He, in fact, endangered the whole city, as the researcher deliberately refused to take any precautions. As before the start of the experiment, he received and visited patients, his secretions were not disinfected, thereby carrying billions of cholera vibrios into the city sewer, and if this whole story had happened with full-fledged bacilli, then an epidemic would probably have broken out in Munich with lightning speed monstrous strength. But these were microbes stripped of their power. Koch later suggested that Pettenkofer was deliberately sent an old, weakened culture, since it was suspected that he intended to conduct the experiment on himself. But, on the other hand, it was not possible to refuse the request of the university department, with which friendly relations were maintained. The request was granted, but as a precaution, the old culture was sent. Nevertheless, this does not in the least detract from the greatness of Pettenkofer's heroic deed.
And other researchers have done this experiment, testing the effects of cholera bacilli on themselves. In this connection it is necessary to mention first of all some Russian researchers. This was done in Paris by a follower of Pasteur, Ilya Ilyich Mechnikov, and after him, Nikolai Fedorovich Gamaleya, Daniil Kirillovich Zabolotny and Ivan Grigorievich Savchenko, who later became a famous Kyiv bacteriologist.
In 1888, Gamaleya was the first to propose the use of dead cholera bacilli to protect against cholera. He tested their harmlessness first on himself, and then on his wife. Zabolotny and Savchenko accepted, in the presence of a commission of doctors, a one-day, that is, fully effective, culture of cholera bacilli; the day before the experiment, each of them subjected himself to immunization by swallowing a culture of killed bacilli. This experiment, which is a continuation of the experiments described above, was carried out in 1897. It is of particular importance in the history of medicine, since for the first time it was proved that infection can be protected not only by injecting the appropriate pathogen, but also by ingesting a weakened culture of bacilli. That is why subsequent experiments in this direction were of such great importance.
The name of Vladimir Khavkin should also be mentioned. Later he became a major bacteriologist. Without prejudice to health, Khavkin injected himself first with a small dose of weakened cholera bacilli, and then a larger one. The result of these no less dangerous experiments was the conclusion that persons who do not suffer from cholera can also be carriers of live, virulent cholera vibrios. So, these experiments were a contribution to the problem of bacillus carriers, which is important not only for cholera, but also for other infectious diseases, for example, for typhoid.
Among the experiments that the researchers set on themselves, one conducted by Mechnikov proceeded very dramatically. Then in France, namely in Brittany, a cholera epidemic raged, supplying material for experiments. Mechnikov, who received the Nobel Prize in 1908 for his bacteriological research, swallowed a large amount of "cholera commas" and remained healthy.
The example of Mechnikov was followed by his assistant Latapi. The result was the same, namely, negative. Then a third of the institute's employees repeated the experiment and swallowed cholera vibrios. This was Dr. Jupil. The result was terrible. He fell ill with cholera in such an acute form that his recovery was in doubt. Mechnikov was deeply shocked. He repeatedly repeated that if Jupil died, he would commit suicide, and probably the threat was not just a phrase. Fortunately, Jupil survived.
In general, it should be stated that of the many self-experiments conducted by scientists at that time and later - forty such experiments are known with the causative agent of cholera - not a single one ended in death, while an accidental laboratory infection at the Hamburg Institute of Hygiene caused death. scientist-researcher Orgel. Of course, it was not always possible to explain why these experiments on oneself ended happily. One can only thank the occasion that contributed to this. Mechnikov was probably right, who put the decision of the question of which of the two people, ceteris paribus, will get cholera, depending on the characteristics of the bacteria that have settled in the intestines of a person, on his intestinal flora. It can perhaps be argued that Mechnikov was a specialist in intestinal bacteria. He divided them into favorable cholera infection and preventing its development. This explanation, of course, is quite acceptable, since it is known that there are wars between bacteria, that they compete with each other, that sometimes one kind of bacteria destroys another. The discovery of penicillin was based precisely on this fact.
Pettenkofer survived his heroic experiment by several years. In February 1901, he shot himself, haunted by a morbid fear of impending decrepitude. Then, probably, they said that it would be better for him if he did not go through his experience.
cholera clinic. The incubation period lasts from 6 hours to 6 days. Cholera begins with diarrhea. The urge to defecate appears suddenly, usually painlessly. The stools are initially fecal in nature, and subsequently acquire a liquid character, may resemble rice water; odorless, but sometimes there is a peculiar smell of dampness, fish. The patient feels weakness, moderate thirst, dry mouth.
Perhaps rumbling at the navel or lower abdomen. Physical and chemical parameters of blood remain normal. Within 1-2 days, often spontaneously, recovery occurs. The above clinical symptoms correspond to patients with dehydration of the 1st degree (cholera enteritis), appear in 40-60% of cholera patients and are recorded more often during the height and recession of an epidemic outbreak. Fluid loss is from 1 to 3% of body weight.
Stage 2 is dehydration with fluid loss from 4 to 6% of body weight. After a few hours or a day, repeated vomiting joins the diarrhea, sometimes with a fountain, without nausea (cholera gastroenteritis develops). Vomit quickly loses its characteristic appearance, becomes watery and also resembles rice water. Profuse diarrhea develops with a frequency of stools up to 15-20 times a day, which lose their fecal character.
Dehydration sets in quickly. Patients complain of weakness, dry mouth, thirst, dizziness. The skin is dry, pale, often with unstable cyanosis, hoarseness of the voice, sometimes spasms of the calf muscles. Skin turgor becomes reduced (the fold straightens slowly). Facial features are sometimes pointed, shadows under the eyes. Blood pressure is lowered (100 mm Hg and below), diastolic is not lower than 40 mm, moderate tachycardia (up to 100 in 1 min.). Possible transient oliguria
3 degree of dehydration corresponds to fluid loss from 7 to 9% of body weight. The onset of the disease is acute, with a rapid increase in symptoms, repeated vomiting, very frequent bowel movements, sometimes in the form of "rice water", significant thirst, constant dizziness, fainting, severe weakness, the temperature is often normal. There are tonic convulsions.
These symptoms are supplemented by acrocyanosis, a decrease in skin turgor (the fold straightens slowly). The features of the patient's face are sharpened, the eyes sink, dark circles appear under the eyes (a symptom of "dark glasses"), the look is suffering, the voice is hoarse, sometimes only a whisper. Increases hypovolemia, hypoxia, thickening of the blood leads to hemodynamic disorders.
The patient's behavior becomes restless (fear of death), sometimes there is excitement. BP goes down. Systolic pressure is 80-60 mm Hg. Art., diastolic pressure may not be determined, the pulse is weak, thready, 120-130 or more beats per 1 minute. Mucous membranes are dry, tachypnea (up to 30 or more in 1 minute), oliguria, often anuria.
The mass of circulating blood plasma decreases to 33 ml/kg, extrarenal azotemia increases. Neutrophilic leukocytosis is observed in the blood, ESR is accelerated. At this stage, the clinical symptoms correspond to manifestations of hypovolemic shock.
Dehydration of the 4th degree, or cholera algid, is decompensated dehydration with fluid loss of up to 10% or more of body weight. This form is observed during outbreaks of cholera in 8-15% of patients. The patient's condition deteriorates sharply. All symptoms of dehydration are markedly pronounced. Hypovolemic shock progresses. Due to intestinal paresis, diarrhea and vomiting may temporarily decrease or even stop, but sometimes they resume against the background of rehydration or after it has ended.
Due to severe hemodynamic disturbances and spasm of peripheral vessels in patients with cholera, coldness of the extremities and skin of the trunk occurs. The skin is not only cold, but sometimes covered with sticky sweat. Body temperature drops to 35 degrees or to 31 degrees (“cadaveric temperature”).
The skin is pale, gray; acquires a marble pattern, loses its elasticity, wrinkles, does not straighten out when assembled into a fold; wrinkles appear on the palms ("the laundress's hand"). The facial features are sharpened, the eyes sink (facies cholerica), the lips, the tip of the nose, the auricles become cyanotic. In some areas (back, buttocks, if the patient is lying on his back), bluish spots appear (due to blood metastases).
The tongue is dry, covered with a grayish coating. The mucous membranes of the oral cavity are dry. The voice is quiet, up to complete aphonia, due to dryness and non-closure of the vocal cords, their convulsive contraction. The expressed tachycardia, pulse on peripheral vessels and the ABP are not defined. Pericardial friction rub is detected. The patient is in deep prostration.
Breathing is shallow, frequent, uneven. Dehydration, hypokalemia, acidosis can cause seizures. Convulsions of a tonic nature extend to all pectoral muscles, including the diaphragm, which leads to hiccups. There may be generalized convulsions - opisthotonus (as in patients with tetanus). The severity of tachycardia, shortness of breath, and a drop in blood pressure correlate with the degree of dehydration and metabolic disorders.
If timely treatment is not carried out, a phase of asphyxia sets in, cholera coma and death against the background of loss of consciousness, severe hemodynamic disturbances, convulsions.
The reactive period (recovery) in patients with cholera can occur against the background of dehydration of any degree, including algida. This period is characterized by a gradual extinction of the acute manifestations of the disease, the patient's skin acquires a normal color, warms up, the pulse approaches normal, blood pressure rises, the voice becomes stronger, urine appears to polyuria; within 2-3 days the body temperature returns to normal. Such reverse changes in most cases occur during intensive care.
Atypical forms of cholera.
Among these forms, severe is fulminant (fulminant), when all its clinical manifestations increase so rapidly that only a few hours pass from the moment the first symptoms appear to hypovolemic shock and death.
Dry cholera.
This is a form when death occurs in the presence of phenomena of circulatory and respiratory failure without diarrhea and vomiting. Clinical manifestations are characteristic of hypovolemic shock, the intestines are filled with fluid, but diarrhea does not have time to develop due to the rapid onset of intestinal paresis and circulatory disorders. This course is very difficult to diagnose, it is observed in very weakened, emaciated individuals.
Hemorrhagic cholera.
It can be with some somatic diseases of the liver, blood vessels, digestive tract (peptic ulcer, ulcerative colitis) when blood impurities appear in the feces and vomit (stools look like meat slops). This gives reason to some clinicians to distinguish hemorrhagic cholera as a special variant of the course of cholera. Similar manifestations can be with mixed infection (cholera + shigellosis). The severity of the course of the disease is affected by dysbacteriosis, chronic alcoholism, diabetes and others.
Erased cholera.
Vibrio cholerae can also be detected in individuals who did not have bowel dysfunction (“asymptomatic vibrio carriers”). But an increase in their sera of vibriocidal antibodies testifies more in favor of a subclinical (erased) infection.
Vibrio carrying.
Clinical recovery in time does not always coincide with the cleansing of the body from the pathogen. Sometimes this process can be delayed for 2-3 weeks, which necessitates dispensary monitoring of people who have been ill (carriers are convalescents).
There are cases of infection with Vibrio cholerae of the gallbladder, which requires duodenal sounding followed by bacteriological examination of bile.
A particularly severe course is observed in children and the elderly, in which the mortality rate reaches 20-40% or more.
Features of the modern course of cholera associated with the specificity of the vibrio El Tor. Cholera caused by this pathogen has a predominantly milder course. Erased and atypical forms with prolonged post-infectious or healthy vibrio carrying are more often observed.
Complications.
They can occur at different stages of the disease, but with the rapid course of cholera, they cannot always be recognized in time. Hypovolemic shock is often considered not as a complication, but as a variant of the severe course of cholera - this is the main criterion for severity.
Acute renal failure occurs in the presence of 3-4 degrees of dehydration, especially against the background of irrational therapy. Long-term infusion therapy, carried out by puncture of the cubital veins or veins of the leg, can lead to the formation of phlebitis, pyrogenic reactions, hypostatic pneumonia, and the like.
This is an acute bacterial disease with an alimentary transmission mechanism, which is characterized by dyspeptic syndrome with severe dehydration.
Historical reference
The first mention of cholera appeared in the writings of ancient times. Hippocrates mentioned the symptoms characteristic of cholera in his writings. For the first time, a pure culture was isolated and studied by the German microbiologist Robert Koch in 1906. Cholera has claimed millions of lives throughout the history of mankind and accompanied all sorts of catastrophes and cataclysms (earthquakes, floods, wars). To date, isolated cases of cholera are recorded in disadvantaged areas of India. The causative agent of cholera was found in the water of the Sea of Azov.
Etiology
The causative agent of cholera is Vibrio cholerae (Vibrio cholerae). This bacterium belongs to the genus of intestinal bacteria, curved (hence the name - vibrio), mobile, has flagella, spores and capsules does not form. There are 2 subspecies of Vibrio cholerae:
- classic - Vibrio cholerae classica;
- El Tor - Vibrio cholerae eltor.
The causative agent of cholera secretes endotoxin during the death and destruction of the bacterial cell and heat-labile exotoxin - cholerogen, which causes dehydration of the body.
Vibrio cholerae is quite stable in the external environment in the presence of liquid. In wastewater, which have an alkaline environment, it can actively multiply. The El-Tor cholera subspecies is more resistant than the classical vibrio. Drying, exposure to direct sunlight, boiling, disinfectants, acidic environment are detrimental to the microorganism.
Epidemiology
Cholera is an anthroponotic infection, that is, its source is only a sick person or a bacteriocarrier. The causative agent is excreted from the body of a sick person from the first days of the disease with feces and vomit during vomiting. Of particular epidemiological danger are bacterial carriers and patients with an erased form of the disease who do not seek medical help and continue to isolate vibrio cholerae into environment.
The mechanism of infection transmission is alimentary with water transmission. Outbreaks of cholera accompany poor sanitation during disasters, wars, natural disasters. There is a summer-autumn seasonality of the disease, which is associated with favorable conditions in the external environment, under which Vibrio cholerae can multiply in wastewater, sewers and reservoirs. Cholera outbreaks have been observed in pipeline accidents in which sewer water enters the water supply.
The mechanism of development of the disease in cholera
The entry gate of infection is the human gastrointestinal tract. At the same time, a significant part of the bacteria dies in the stomach, due to the action of hydrochloric acid. However, with reduced stomach acidity, bacteria survive and enter the small intestine, where the alkaline environment is favorable for their reproduction. Here, Vibrio cholerae actively secretes exotoxin - cholerogen. It leads to the reverse secretion of fluid and salts from the blood into the lumen of the small intestine, which leads to such disorders:
- decrease in circulating blood volume;
- thickening of the blood, which disrupts the functioning of the kidneys and develops acute renal failure;
- a decrease in the content of salts in the body, especially potassium and sodium, which leads to disturbances in the activity of the nervous system and heart rhythm;
- hypovolemic shock is an extremely serious condition associated with a critical decrease in free fluid and salts in the body, without adequate treatment can lead to death.
After the illness, an unstable and short-lived type-specific immunity to the cholera pathogen develops.
Clinical picture of cholera
The incubation period lasts from several hours to 5 days. Depends on the number of bacterial cells of vibrio cholerae that have entered the body. The most characteristic symptoms of infection are vomiting, diarrhea, and dehydration.
Features of vomiting, allowing to suspect cholera:
- occurs suddenly, without previous nausea;
- does not alleviate the patient's condition;
- vomiting of a large amount of odorless liquid and food residues (may be at the very beginning of the disease) - “vomiting a fountain”.
Also, diarrhea with cholera has distinctive features:
- diarrhea develops without abdominal pain (the main difference from other intestinal infections);
- there are no fecal stools (they can only be at the beginning of the disease), the stool is a clear, odorless liquid;
- on the 2-3rd day (sometimes on the 1st) of the disease, the stool acquires the characteristic appearance of "rice water" - a clear liquid with lumps of white mucus (dead cells of the epithelium of the mucous membrane of the small intestine).
Symptoms of dehydration in cholera are:
- decrease in turgor and elasticity of the skin - when collecting the skin into a fold, it straightens out within 0.5 - 1 minute (normal - immediately);
- "Laundress's hands" - wrinkling of the skin of the palms of the hands (occurs with laundresses when their hands are in the water for a long time);
- violations of the central nervous system (associated with the loss of salts) - manifested by a violation of consciousness, up to coma;
- a sharp decrease in diuresis - rare urination with a reduced amount of urine, while the urine is dark, concentrated.
There are several forms of cholera:
- typical form - the main symptoms are present - vomiting and diarrhea;
- atypical form - there may be no vomiting or diarrhea;
- erased form - characterized by one-time vomiting and diarrhea, dehydration does not develop, the infected person feels well, does not seek medical help (epidemiologically dangerous form);
- cholera algid - a severe variant of the course of cholera, after a few hours, continuous vomiting and diarrhea develop, dehydration, body temperature drops to 34-35 ° C, hypovolemic coma and death occur in a few days;
- lightning-fast form - several hours pass from the appearance of the first symptoms to the development of hypovolemic shock;
- dry form - noted fast development dehydration, while vomiting and diarrhea are not expressed.
The severity of cholera depends on the degree of dehydration (dehydration) of the body:
- I degree - dehydration is not expressed, water loss is 1-3% of body weight, there are no changes in the nervous system and heart;
- II degree - water loss is 4-6% of body weight, there may be slight changes in the nervous system (irritability) and heart (arrhythmia);
- III degree - 7-9% of body weight is lost of water, severe dehydration, confusion appears on the part of the nervous system, convulsions are possible, severe arrhythmia, the development of renal failure begins;
- IV degree - very severe dehydration, water loss of more than 10% of body weight, consciousness is absent, hypovolemic coma develops, severe renal failure.
In children and the elderly, the course of cholera is more severe.
A complication of cholera can be cholera typhoid, which develops as a result of the penetration of other microorganisms from the intestine into the blood against the background of a decrease in immunity. Manifested by the fact that against the background of the symptoms of cholera, general intoxication joins with an increase in body temperature to 39-40 ° C, this significantly aggravates the course of cholera.
Diagnosis of cholera
The main methods are bacteriological and microscopic. With the bacteriological method of diagnosis, the material (vomit, feces, food debris, water) is collected in sterile dishes and inoculated on alkaline nutrient media. After the growth of cultures, biochemical and serological (using antibodies) identification of bacteria is carried out. The result is obtained in 24-48 hours. Material microscopy is an express method for diagnosing cholera. A positive result is considered when curved rod-shaped bacteria are detected, which are located in a smear in the form of a flock of fish.

Treatment
It is carried out only in the conditions of an infectious diseases hospital in compliance with anti-epidemic rules (thorough disinfection of feces and vomit, the work of medical personnel in anti-plague suits).
Unlike other infections, with cholera, pathogenetic therapy aimed at rehydration (restoration of lost fluid and salts) comes to the fore:
- oral rehydration - the patient drinks the proper amount of saline solutions (rehydron), oral rehydration is effective only in the absence of vomiting;
- intravenous rehydration - involves the intravenous administration of saline solutions containing salts of potassium, sodium, calcium, etc.
Rehydration is stopped only in the absence of vomiting and the predominance of urination over diarrhea for 12 hours.
The earlier measures are taken to restore the volume of fluid and salts in the body, the better the prognosis of the disease will be.
Etiotropic therapy is carried out to destroy the vibrio cholera in the patient's body. For this, antibiotics are used - doxycycline, less often ciprofloxacin or furazolidone (in case of resistance of the pathogen to doxycycline).
An extract from the hospital is carried out after the disappearance of the symptoms of cholera and 3 negative bacteriological results of the study of the material from the patient. Workers in the food industry and the water supply system are examined 5 times with an interval of 24 hours. After discharge, people who have had cholera are registered in the sanitary-epidemiological station and in the office of infectious diseases at the place of residence, where observation is carried out for 3 months. During the first month, a bacteriological examination of feces for the presence of cholera vibrio is carried out 1 time in 10 days.
cholera prevention
Includes non-specific prophylaxis and anti-epidemic measures, in case of detection of a patient or a bacteriocarrier.
Nonspecific prophylaxis of cholera is:
- personal hygiene rules - washing hands after visiting the restroom, before eating;
- you can’t drink water from unknown sources, especially from abandoned wells, reservoirs, but if it’s not possible, then you need to boil the water and add a little citric acid to it (the vibrio cholerae dies in an acidic environment).
Anti-epidemic measures are aimed at preventing the spread of cholera in the case of an identified patient or bacteriocarrier and include:
- hospitalization of a patient in a cholera hospital (deployed in an infectious diseases hospital);
- isolation and treatment of the patient in a separate box;
- placement of contacts (relatives, cohabitants of the patient) in a separate isolation ward with an observation period of 5 days;
- deployment of a provisional hospital, where patients with dyspeptic syndrome are observed until the diagnosis is fully established;
- contact people are given emergency prophylaxis of cholera, for which antibiotics (doxycycline) are used;
- carry out vaccination in the focus of the disease - corpuscular cholera vaccine and cholerogen-toxoid, immunity after vaccination persists for 4-6 months.
To limit and eliminate the source of cholera, the following measures are taken:
- restriction of entry and exit to an unfavorable territory;
- door-to-door rounds in order to identify patients;
- identification and isolation of people who have been in contact with cholera patients, as well as with contaminated environmental objects;
- current and final disinfection.
Since cholera is classified by the World Health Organization as a particularly dangerous infection, compliance with anti-epidemic rules is regulated in the country at the legislative level, so patients who refuse hospitalization and isolation are responsible.
It is important to remember that at the present stage, cholera is successfully treated, but only if you seek medical help early for adequate pathogenetic and etiotropic treatment.
Other especially dangerous infections.
Cholera is an infectious disease that primarily affects the gastrointestinal tract. Affecting the gastrointestinal tract, cholera causes severe damage to the body. This is manifested in severe exhaustion and dehydration of a person. As a result, the mortality rate from this disease reaches 50%. The most important thing is to recognize the disease in time and start treatment immediately. Therefore, let's talk in more detail about what cholera is, the clinic, diagnosis, prevention, and treatment of an infectious disease at the present time.
Pathogen
Any infectious disease has its pathogen. Cholera is caused by Vibrio cholerae. This bacterium has the appearance of a slightly curved rod, at the end of which is a flagellum. Thanks to the flagellum, Vibrio cholerae can move very quickly and travel long distances.
Route of infection
Human infection occurs by the fecal-oral route. Infection can occur when drinking large amounts of raw and bacteria-contaminated water, as well as unwashed vegetables, fruits, etc. The main role in such cases is played by the number of swallowed bacteria and the state of the organism as a whole. If a person is healthy and does not have diseases of the gastrointestinal tract, then the dose of ingested bacteria should be very large.
Hydrochloric acid can kill a lot of vibrios, but if a person suffers from gastritis or other diseases of this type, then the risk of developing cholera increases hundreds of times. In addition, infection can occur through unwashed hands, and by eating shellfish from contaminated water bodies, as they are able to accumulate bacteria in their bodies.
Usually the spread of cholera occurs in a certain circle of people who eat the same foods. In this group there are carriers who may not have any symptoms of the disease, but it is they who release a huge amount of vibrios into the environment. In addition, bacteria get on food and into the soil from the vomit and feces of sick people. In this case, this group of people is isolated in order to prevent further spread of the disease.
Clinic
Like any infection, cholera has its own incubation period. The duration of the incubation period is different for each person: from several hours to several days. At this time, a critical amount of bacteria accumulates in the body.
When pathogens enter the human small intestine, the acute phase of the disease begins. This phase is characterized by very severe diarrhea, which is not accompanied by pain in the abdomen.
The number of acts of defecation can reach 30 times a day. At first, the feces are liquid or mushy, and then become colorless with flakes floating in them. In addition to diarrhea, a person suffers from severe vomiting. First, the vomit contains semi-digested foods, and then in the form of "rice water". Vomiting is not preceded by nausea. With such severe diarrhea and frequent vomiting, the human body quickly loses water.
There is severe dehydration, dry mucous membranes, sunken eyes, reduced skin turgor. The disease is accompanied by convulsions, cardiac arrhythmias and lack of urine. There is a very strong depletion of the body. And the most important symptom is a normal or slightly reduced body temperature. This is what distinguishes cholera from other infectious diseases.
If therapeutic measures do not begin within 12 hours, the person dies.
But this is a severe form of cholera. There is a hidden form. In this case, a person may not have all of the symptoms listed, but he will be a carrier and infect other people.
Diagnostics
Diagnosis of cholera is not difficult. Sometimes, bacteriological confirmation is not even required, since a vivid clinical picture makes it easy to make an accurate diagnosis.
Treatment
The treatment of cholera is based on replenishing the water lost by the body. Next, the balance of electrolytes in the body and further rehydration are carried out.
The drugs used for this are administered as electrolyte solutions into a vein, and some of them are taken by patients in the form of tablets. The required amount of vitamins and nutrients is also restored. Along with these actions, the destruction of cholera vibrios also occurs. This therapy is also not difficult, because the bacterium is sensitive to conventional tetracycline. Rehabilitation therapy and a course of antibiotics will quickly put a person on his feet. But the most important thing for today remains to reduce the number of cases of the disease.
Prevention
Prevention of cholera is carried out at the state level. But all sanitary measures will not be effective if the person himself does not follow elementary security measures. To prevent infection with Vibrio cholerae, you must wash your hands thoroughly, do not drink unpurified water, buy food only in a safe place and avoid swimming in prohibited places. Take care of yourself! Finally, the cholera poster: click to enlarge the picture and then click a second time in the lower right corner to enlarge it even more.